Xylazine, also known as “tranq,” is a non-opioid drug commonly used for veterinary purposes which has been showing up more frequently in the illicit drug supply. To address the significant health challenges caused by xylazine, Governors have begun to implement a variety of policy solutions, ranging from bolstering drug checking initiatives to scheduling xylazine as a controlled substance at the state level.
The Food and Drug Administration (FDA) has not approved xylazine for human use and it is currently not a controlled substance. However, according to the Congressional Research Service, xylazine is subject to regulation by the FDA and some state laws. Since 2019, xylazine has become an adulterant in the illicit drug supply and is increasingly being detected in fatal overdoses in several cities in the United States.
Frequently seen in combination with other drugs, xylazine is known to lengthen the effects of fentanyl, which now comprises much of the illicit opioid supply. It is currently unclear how xylazine is primarily entering the illicit drug supply; however, sources report that there is little evidence of significant diversion from veterinary sources.
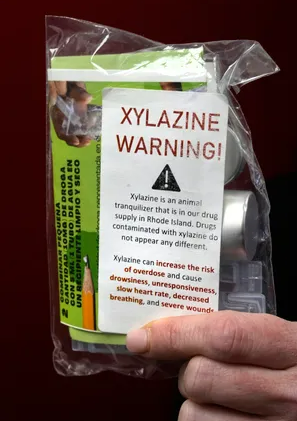
Xylazine is a particularly dangerous drug supply contaminant for several reasons. As it is not an opioid, opioid overdose reversal drugs such as naloxone (e.g., Narcan) will not reverse the effects of xylazine. Xylazine has sedating/depressing effects on the respiratory system, which compound the respiratory depressive effects of opioids like fentanyl. In cases of a combined xylazine and opioid overdose, overdose reversal drugs (e.g., naloxone) should still be used to reverse the opioids’ effects; however, rescue breathing and contacting emergency medical services are crucial to ensuring the individual’s recovery since overdose reversal drugs will not counteract the effect of xylazine. Rapid patient response and regaining consciousness after naloxone administration may be less frequent than overdose responders have come to expect with those who have ingested opioids.
Xylazine is also known to cause skin and soft tissue wounds, abscesses and ulcers which are often severe enough to require hospitalization and amputation. People who use substances adulterated with the drug, whether knowingly or unknowingly, may also develop dependence and experience withdrawal symptoms unique to xylazine and different from opioid withdrawal. Xylazine withdrawal has unique clinical considerations that many providers are not yet prepared to address. As a result, many patients abandon substance use treatment early when insufficiently managed withdrawal symptoms become unbearable.
State Responses
In most states, public health departments and other state administrative agencies have issued alerts and communications about xylazine. These communications generally fall into two categories: alerts/press releases for the purposes of awareness and public health information/risk reduction messaging for providers as well as people who use substances.
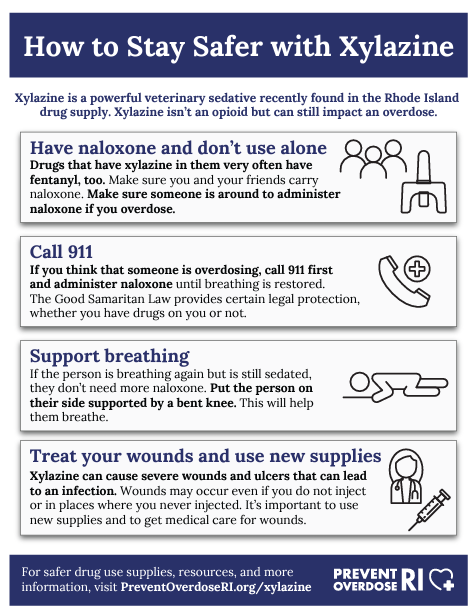
In addition to general awareness of prevalence and dangers, state communications have included clinical considerations and overdose response information for healthcare providers and overdose responders. For example, some states are providing information about responding to overdoses involving xylazine, prevalence of wounds in people using the drug and withdrawal in those dependent on it. The Substance Abuse and Mental Health Services Administration (SAMHSA) issued a letter on March 27, 2023, addressing some of these considerations. Some specific state examples include:
- Iowa – The Iowa Governor’s Office of Drug Control Policy created a brief website to inform the public about xylazine, with links to the federal resources provided by the Drug Enforcement Agency (DEA), National Institute on Drug Abuse (NIDA) and the Food and Drug Administration (FDA.)
- Rhode Island – Information materials on xylazine were provided to the public through the “Prevent Overdose RI” initiative organized by the Rhode Island Governor’s Overdose Prevention and Intervention Task Force.
- Vermont – On August 31, 2022, Vermont Governor Phil Scott issued a proclamation to create an Awareness Day, recognizing the increase in overdose related to fentanyl, xylazine and other substances.
Several state legislatures have also introduced bills related to xylazine. This includes listing xylazine as a scheduled drug and creating testing requirements for xylazine during toxicology screenings. Governors and legislators can classify xylazine as a scheduled drug using authority provided to them in their state’s statutory law defining controlled substances. Although these laws generally mirror the federal Controlled Substances Act (CSA), state policy may deviate from this standard as long as the changes do not conflict with the federal policy, as defined by federal preemption standards in this area. Furthermore, state statutes or regulations frequently include language that provides flexibility and permits a Governor or state agency to make alterations to drug schedules in extraordinary or emergency circumstances.
Governor’s offices have also responded to xylazine through various executive actions. Specific examples include:
- Ohio – On March 29, 2023, Ohio Governor Mike DeWine issued an executive order directing the State Board of Pharmacy to classify xylazine as a Schedule III controlled substance. (Warning: executive order contains images of xylazine-related wounds.)
- Pennsylvania – On April 18, 2023, Pennsylvania Governor Josh Shapiro announced the state would be submitting a notice of intent to temporarily classify xylazine as a Schedule III drug. Pennsylvania also submitted a notice of intent to schedule nitazines, a class of synthetic opioids, as a Schedule I drug.
- West Virginia – On March 29, 2023, Senate Bill 546 passed the legislature and was signed into law by West Virginia Governor Justice to classify xylazine as a Schedule IV drug.
- Florida – Xylazine is listed as a scheduled drug under Florida Stat. 893.03 (Standards and schedules).
Other actions states have taken include changing policy to decriminalize drug checking equipment and enhanced detection of emerging adulterants in the drug supply. States vary in legality of drug checking equipment, which includes supplies such as fentanyl test strips. Fentanyl test strips have been widely distributed to people who use drugs to detect fentanyl and have a demonstrated association with risk reduction behavior change. As of August 2022, 22 states and the District of Columbia had laws permitting drug checking equipment broadly, and eight additional states had laws allowing for drug checking equipment for fentanyl and/or synthetic opioids only. Several more states have pending legislation or passed new legislation in 2023, including Ohio and South Dakota. States with policies that have decriminalized or legalized drug checking equipment broadly (not fentanyl-specific), may be well-poised to take advantage of xylazine test strips, which have recently become available and are not yet widely distributed. Several states also have more extensive drug checking programs that inform the public of the prevalence of xylazine and other emerging substances in the drug supply; these states include Maryland, Massachusetts and North Carolina.
As aforementioned, severe wounds are another harmful consequence of xylazine prevalence, so state investments in trusted community programs providing low barrier wound care may also help combat the impacts of xylazine. Many street outreach and harm reduction programs offer wound care services, with varying levels of care ranging from distributing wound care supplies to nurse consultations for wounds on-site. For example, New Jersey’s ARCH program staffs each Harm Reduction Center with a nurse who is available to provide wound care in addition to many other services. These types of programs that engage people who use drugs may serve as a key entry point and connection to other services, including substance use disorder treatment.
Federal Responses
To respond to the recent increase in overdoses involving xylazine, federal agencies have issued various communications around xylazine, including the following:

- On September 17, 2021, the Centers for Disease Control and Prevention (CDC) published two “Notes from the Field” discussing the detection of xylazine and its role in drug overdoses in populations throughout the United States and in Connecticut.
- On November 8, 2022, the FDA released a statement acknowledging the presence of xylazine in illicit drugs and warning of the risks.
- On January 18, 2023, the White House Office of National Drug Control Policy (ONDCP) hosted a meeting of the Biden Administration’s Evolving and Emerging Threats Committee, during which members discussed the emergence of fentanyl adulterated with xylazine in the illicit drug supply.
- On February 28, 2023, the FDA issued an import alert for drugs containing xylazine that are or appear to be adulterated or misbranded.
- On March 20, 2023, the Drug Enforcement Administration (DEA) released a public safety alert to communicate the widespread threat of fentanyl mixed with xylazine.
- On March 27, 2023, SAMHSA released a letter to providers and grantees detailing the risks of xylazine.
- On April 12, 2023, Dr. Rahul Gupta, Director of the White House Office of National Drug Control Policy (ONDCP), released a statement which officially designated fentanyl adulterated or associated with xylazine as an emerging threat to the United States. The Biden Administration will publish a national response plan to address xylazine which will include information on xylazine testing, treatment and care protocols, data systems, strategies to reduce the supply and research.
The recent increases in detection of xylazine has also spurred Congressional action. Proposed legislation in the current session includes the TRANQ Research Act. This bill would require the National Institute of Standards and Technology (NIST) to conduct research into xylazine, including additional methods for detection and responsible handling of the drug. The Combating Illicit Xylazine Act was also introduced, which would list xylazine as a controlled substance and create penalties for unlawful use and distribution of xylazine under the Controlled Substances Act (CSA).
For more information on this topic, or to request technical assistance related to this issue area, please contact Ken Hardy (KHardy@nga.org) or Marianne Gibson (MGibson@nga.org)