
Maternal and Infant Health
While the United States is a high-income country with advanced medical facilities, the state of maternal health in the US is a matter of concern.
Tackling the Maternal and Infant Health Crisis: A Governor’s Playbook
Dear Partners,

Over the past year, many of us have traveled across the country to learn more about our national maternal health crisis, a journey that we in New Jersey began in 2018 as a first step to face our home state’s unacceptable racial disparities in maternal and infant health outcomes.
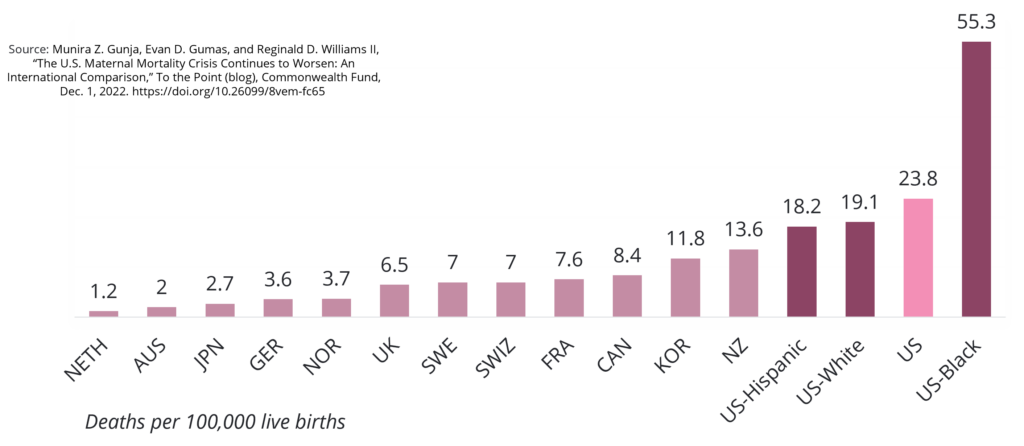
As the wealthiest country in the world, the United States should be at the cutting-edge of maternal health care. Every mother and baby across our nation should begin their life together in health, wellness and joy. But tragically – and astonishingly–that is not the case. In fact, the United States has a maternal mortality rate more than double that of other high-income countries like Norway and Germany.
In stark contrast to these disturbing statistics is our shared resolve to end this crisis. In visiting communities across the nation – from Salt Lake City to Los Angeles to Detroit to Philadelphia – we have not only learned more about the causes and consequences of our maternal and infant health crisis, but we have also seen an overwhelming and universal commitment to protecting our mothers and babies. No matter what state we visited or the political, socio-economic, racial, or religious makeup of the community, we saw again and again that ensuring our families begin their lives together intact and healthy is a responsibility in which we all share and to which we are innately connected.
In that spirit, we are thrilled to release the National Governors Association Maternal and Infant Health Initiative Playbook, a guide designed to make transformational change in a system that has historically failed our mothers and babies, especially our Black, Hispanic and American Indian and Alaskan Native mothers and babies. Of course, no one knows the unique challenges of a community better than the members of that community. Therefore, as you utilize this Playbook, we challenge you to start by sitting and listening to those most impacted, the moms and families across your state. And, as you progress in this work, we hope you will continue to collaborate with us to share your successes and amendments such that all of us might move forward together.
Communication and partnership are truly the linchpins of our strategy to improve our maternal and infant health outcomes on a national scale. Ultimately, it will be all of our voices, resources and commitment that together make the United States the safest nation on earth to deliver and raise a baby.
So, I thank you for your shared commitment to every mother and baby across the United States, and I look forward to continuing this work together.
My very best,
Tammy Snyder Murphy
First Lady of New Jersey
2022-2023 Chair of the National Governors Association Spouses Program
Executive Summary
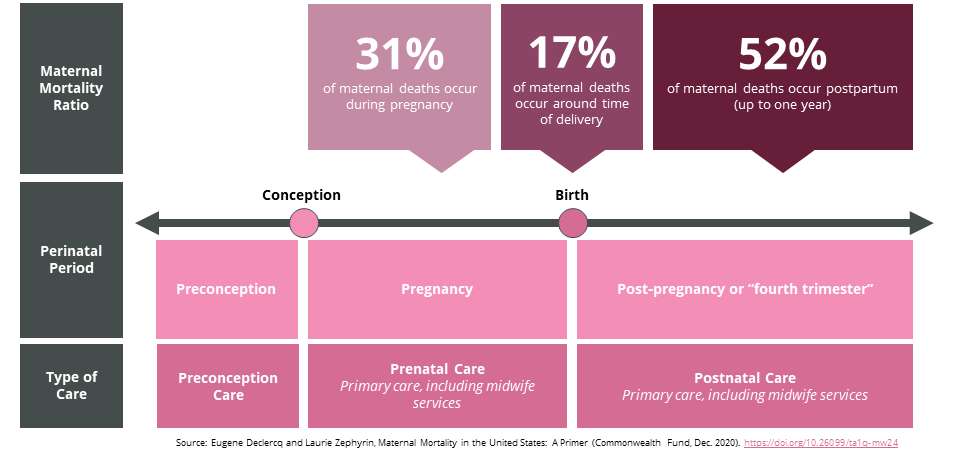
The United States has the worst rates of maternal mortality among developed countries, and the gap between rates in the U.S. and other high-income countries is widening. Despite federal and state funding and attention targeting the issue, poor adverse outcomes persist. Traditionally, interventions to address maternal mortality have focused on supporting labor and delivery; however, maternal risk extends beyond birth with 31 percent of maternal deaths occurring during pregnancy and a staggering 52 percent of maternal deaths occurring post-partum, up to one-year post-birth.
Racial disparities are especially evident for Black and American Indian and Alaskan Native mothers, who are two to three times more likely than white mothers to die from childbirth, even when holding economic and education levels constant. Maternal care in rural communities is also limited as almost 2 million rural women of childbearing age live in maternal care deserts, where there are no obstetric services within a county of residence. There are also heavy financial costs associated with high rates of maternal mortality and untreated perinatal mental health conditions with some estimates of the associated costs as high as $32.3 billion per year from conception through the child’s fifth birthday.
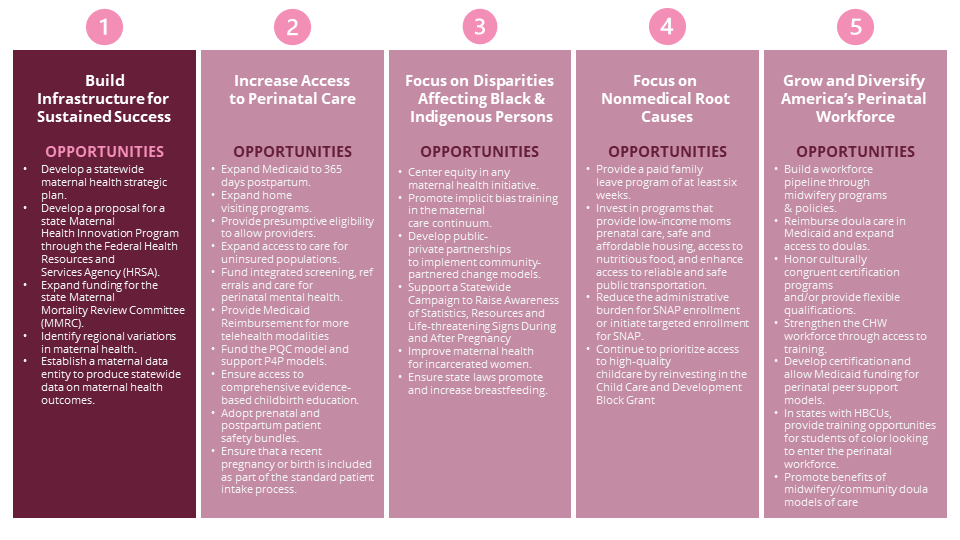
Despite the prevalence of these poor outcomes, the majority of maternal deaths are preventable. Many states are already taking action to build more cohesive and aligned approaches to reducing poor birth outcomes. States can play a vital role in advancing and bolstering these efforts, and this report outlines 32 policy recommendations that are already in practice and feasible for state governments to implement.
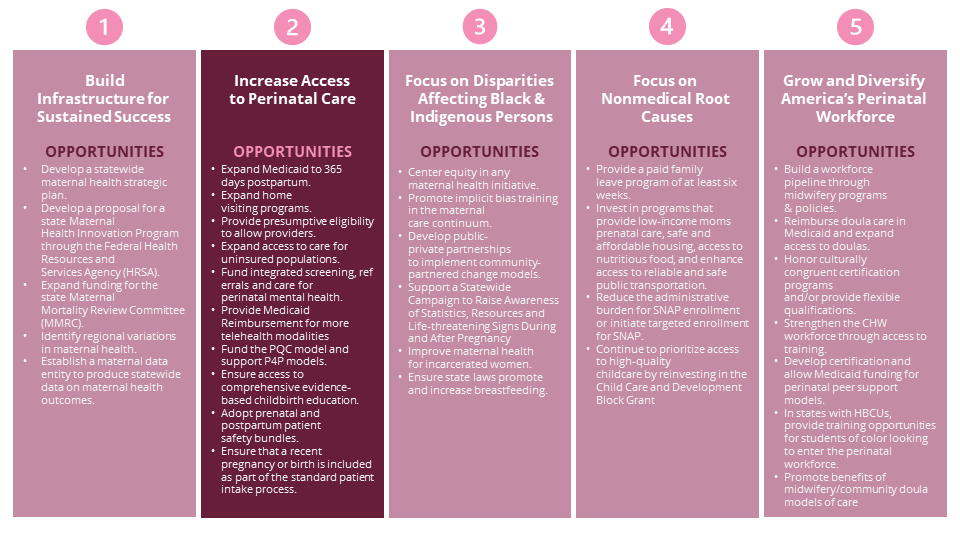
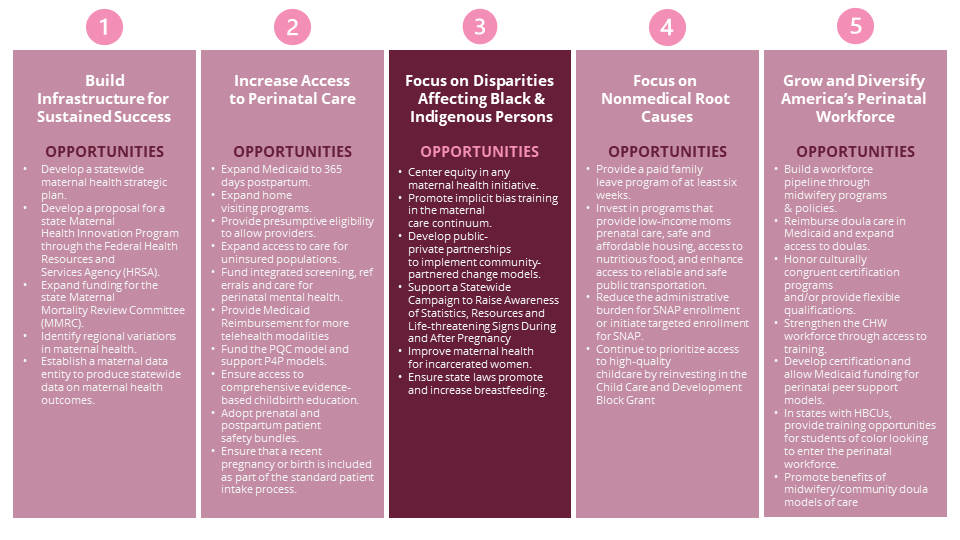
Build Infrastructure for Sustained Success
- Develop a statewide maternal health strategic plan.
- Develop a proposal for a state Maternal Health Innovation Program through the Federal Health Resources and Services Agency (HRSA).
- Expand funding for the state Maternal Mortality Review Committee (MMRC).
- Identify regional variations in maternal health.
- Establish a maternal data entity to produce statewide data on maternal health outcomes.
Increase Access to Perinatal Care
- Expand Medicaid to 365 days postpartum. Expand home visiting programs.
- Provide presumptive eligibility to allow providers to treat pregnant people when they first seek prenatal care rather than waiting until after Medicaid eligibility is reviewed and determined.
- Expand access to maternal and infant care for uninsured populations.
- Fund integrated screening, referrals and care for perinatal mental health.
- Provide Medicaid Reimbursement for more telehealth modalities.
- Fund the PQC model and support P4P models.
- Ensure access to comprehensive evidence-based childbirth education.
- Adopt prenatal and postpartum patient safety bundles.
- Ensure that a recent pregnancy or birth is included as part of the standard patient intake process.
Focus on Disparities in Affecting Black and American Indian and Alaskan Native Persons
- Center equity in any maternal health initiative.
- Promote implicit bias training in the maternal care continuum.
- Develop public-private partnerships to implement community-partnered change models.
- Support a statewide campaign to raise awareness of statistics, resources and life-threatening signs during and after pregnancy.
- Improve maternal health for incarcerated women.
- Ensure state laws promote and increase breastfeeding.
Focus On Non-Medical Root Causes
- Provide a paid family leave program of at least six weeks.
- Invest in programs that provide low-income moms prenatal care, safe and affordable housing, access to nutritious food, and enhance access to reliable and safe public transportation.
- Reduce the administrative burden for Supplemental Nutrition Assistance Program (SNAP) enrollment or initiate targeted enrollment for SNAP.
- Continue to prioritize access to high-quality childcare by reinvesting in the Child Care and Development Block Grant.
Grow and Diversify America’s Perinatal Workforce
- Build a workforce pipeline through accredited midwifery programs and policies that promote midwives.
- Reimburse doula care in Medicaid and expand access to doulas.
- Honor culturally congruent certification programs and/or provide flexible qualifications.
- Strengthen the community health worker workforce through certification and increased access to training.
- Develop certification and allow Medicaid funding for perinatal peer support models.
- In states with Historically Black Colleges and Universities (HBCUs), provide training opportunities for students of color looking to enter the perinatal workforce.
- Promote benefits of midwifery and community doula models of care.
While these recommendations are feasible to implement, they will require careful planning, resourcing and coordination, where relevant, across state agencies, territories and communities, alongside non-profits, philanthropy and the corporate sector. State-level leadership and action is vital to the success of reducing adverse outcomes in maternal health; however, there is no one-size-fits-all approach. In addition, the relationship amongst sovereign Tribal Nations, states and the federal U.S. government underscores the importance of collaborative policy development to address maternal and infant health.
While these recommendations are feasible to implement, they will require careful planning, resourcing and coordination, where relevant, across state agencies, territories and communities, alongside non-profits, philanthropy and the corporate sector. State-level leadership and action is vital to the success of reducing adverse outcomes in maternal health; however, there is no one-size-fits-all approach. In addition, the relationship amongst sovereign Tribal Nations, states and the federal U.S. government underscores the importance of collaborative policy development to address maternal and infant health.
This Playbook presents pathways to consider. States are encouraged to use this toolkit as a guide and ultimately take actions that fit within individual state context and respond to the needs of their communities.
Introduction
Every year, the National Governors Association (NGA) hosts initiatives to inform Governors, spouses and state policymakers on best practices to holistically address critical social and environmental issues across the country. The hosts of the 2022–23 Chair’s and Spouse’s initiatives, New Jersey Governor Phil Murphy and First Lady Tammy Snyder Murphy, focused on youth mental health and maternal and infant health respectively. These two issues pose enduring, national challenges and have been exacerbated due to the COVID-19 pandemic and its aftermath.
This Playbook is a toolkit for immediate action to improve maternal and infant health. Many of the highlighted policies work to address the significant discriminatory policies and practices embedded in organizational structures that lead to disparities in maternal health outcomes, as poor maternal health is a key driver of poor infant health.
First Lady Murphy’s NGA maternal and infant health initiative focused on four key pillars:
- Centering Women’s Voices in Maternal Health Policy
- Improving and Utilizing Maternal Health Data
- Expanding Access to Quality of Care
- Elevating Innovative Maternal Health Policies, Programs and Technologies
The initiative included four stakeholder roundtables focused on each pillar, bringing together Governors and their staffs, experts, individuals with lived experience, philanthropic funders, advocates, nonprofit organizations and companies to identify recommendations. In addition to the roundtable discussions, the NGA maternal health team conducted site visits, extensive research and dozens of interviews to identify promising recommendations and tangible examples from across states with a bipartisan lens.
This Playbook outlines problems and offers evidence-based policy considerations with state-level examples. The 32 recommendations in this report fall into five priority areas and may be implemented in concert with critical stakeholders, such as industry and community leaders, community-based organizations, faith-based organizations and — critically — people with lived experience.
- Build Infrastructure for Sustained Success: State-level strategic planning, reporting, supportive platforms, collaboratives and centers contribute to improved, sustained outcomes for mothers, infants and their families, as well as to increased accountability.
- Increase Access to Perinatal Care: Innovative policies focused on expanding coverage, extending care (including behavioral health services) and integrating technological supports are effectively increasing access to quality and culturally responsive care.
- Focus on Disparities Affecting Black and American Indian and Alaskan Native Persons: Policies, initiatives and implementation plans that intentionally raise awareness of racial disparities in maternal and infant health causes and outcomes are necessary to ensure that mothers and families have access to respectful care.
- Focus on Nonmedical Root Causes: Outside the clinical birthing experience, policies that support paid leave, expand coverage for child care and consider the needs of families with low incomes related to food, housing and transportation significantly contribute to improved health outcomes.
- Grow and Diversify America’s Perinatal Workforce: The current perinatal workforce lacks the capacity and training to meet the needs of all mothers, infants and families, especially historically underrepresented and at-risk communities. Emerging evidence shows that expanding the workforce to professionals who serve patients in nonclinical settings and attend to needs beyond six weeks postpartum can reduce adverse maternal and infant birth outcomes.
NGA MATERNAL HEALTH INITIATIVE SITE VISITS
The year-long NGA Maternal Health Initiative was informed by four roundtables held in Salt Lake City, Utah (October 2022); Santa Monica, California (January 2023); Detroit, Michigan (March 2023); and Philadelphia, Pennsylvania (May 2023). Each roundtable incorporated the lived experience and diversity of participants and had a focus on health equity, illustrating how discussions of policy look and feel in communities across the country. Site visits to local organizations in the cities where the roundtables took place highlighted how policy impacts communities. The following four organizations hosted site visits providing depth and informing policy recommendations.
Sacred Circle Healthcare, Salt Lake City, Utah
Started in 2012 as an entity of the Confederated Tribes of the Goshute Reservation, Sacred Circle Healthcare (SCHC) is owned and operated by the Goshutes and aims to preserve the Goshute heritage of protecting and caring for family through their work with underserved populations in their local communities. SCHC’s Circle of Care™ philosophy centers patient relationships and the Goshute tribe’s tradition of healing. With diverse providers and specialties working together in a single location, Sacred Circle Healthcare provides everything from substance use disorder treatment to pharmacy and dental services, physical therapy, primary care, radiology, mental health and more. The centers serve a broad group of populations that are underserved, including anyone eligible for Medicaid, those without insurance and people of different ethnicities, not just Native Americans.
Black Women for Wellness, Los Angeles, California
Black Women for Wellness (BWW) started as a group of six women who were concerned with the health and well-being of Black babies and, in 1994, teamed up with the Birthing Project as “sisterfriends.” This grassroots program dedicated its time and mission to matching pregnant women with “sisterfriends” — mentors who coached expecting mothers throughout their pregnancy and until the child was at least a year old. These mentorship experiences provided support systems to combat infant and maternal mortality rates. Today, BWW works in Los Angeles County and in Stockton and the San Joaquin Valley in Northern California across a range of program areas, including reproductive justice, civic engagement, environmental justice and wellness.
Birth Detroit, Detroit, Michigan
Birth Detroit is a Black-led birthing center for every birthing person experiencing a pregnancy with no active complications or increased risk for complications — also known as a low-risk pregnancy. Birth Detroit focuses on community-based maternal care by providing prenatal and postpartum care by midwives, as well as childbirth education and postpartum support. Birth Detroit was formed after a 2018-2019 survey found that the community wanted a birthing center that provided prenatal visits, education and full-spectrum support for birthing persons, respecting race, culture, language, gender identities and life experiences.
Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania
Children’s Hospital of Philadelphia (CHOP) is one of the oldest hospitals in the country and has set up systems and practices that have been replicated in children’s hospitals across the country. The Richard D. Wood Jr. Center for Fetal Diagnosis and Treatment was founded in 1995 to specialize in fetal diagnosis, surgery and care. Since its founding, the center has cared for more than 30,426 expectant parents from all 50 states and more than 70 countries. They use a family-centered approach that includes counseling and support services, both throughout the experience and through connections to postnatal care. They diagnose and treat myelomeningocele (spina bifida), congenital heart disease and neurologic abnormalities, among other rare conditions.
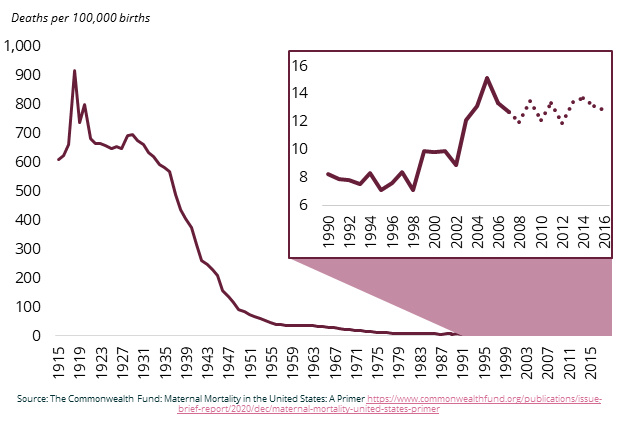
America’s Maternal Health Crisis
The United States has the worst rates of maternal mortality among developed countries, and the gap between rates in the U.S. and other high income countries is widening. The National Vital Statistics System of the Centers for Disease Control and Prevention (CDC) reported that the maternal mortality rate in the U.S. increased from 23.8 maternal deaths per 100,000 live births in 2020 to 32.9 per 100,000 live births in 2021.6F[ii] Despite federal and state funding and attention put toward the issue, adverse outcomes are disproportionately represented among Black and American Indian and Alaskan Native mothers. Traditionally, efforts have focused on supporting labor and delivery; however, maternal risk extends beyond birth and requires a more comprehensive approach to reduce poor outcomes.
Racial and geographical disparities underly these statistics. Racial disparities are especially evident for Black and American Indian and Alaskan Native mothers who are two to three times more likely than white mothers to die from childbirth, even when holding economic and education levels constant. In some states, the disparities are significantly higher. Black infants experience similar disparities in death rates as well. Maternal mortality rates for Hispanic and Latina mothers were previously on par with rates for white mothers but dramatically increased during the pandemic. Maternal care in rural communities is also limited as almost 2 million rural women of childbearing age live in maternal care deserts where there are no obstetric facilities within their county of residence. Further, only seven percent of all obstetric care providers serve rural communities.
Women who are American Indian and Alaskan Native are 4.5 times more likely than non-Hispanic white women to die during pregnancy. Between 2005 and 2014, all Americans experienced a decline in infant mortality except for American Indian and Alaskan Natives who had infant mortality rates 1.6 times higher than the non-Hispanic white population and 1.3 times the national average.
There are heavy financial costs associated with high rates of maternal morbidity and untreated perinatal mental health conditions. Maternal morbidity encompasses physical and psychological conditions resulting from, or influenced by, pregnancy. These conditions do not necessarily lead to death, but they can have a negative impact on quality of life that lasts for months, even years. A 2019 Commonwealth Fund study found evidence among nine maternal morbidity conditions, such as hypertensive disorders, and 24 maternal and child outcomes, such as cesarean section delivery and preterm birth. In 2019, these maternal morbidities and negative maternal and child outcomes resulted in an estimated total for all U.S. births of $32.3 billion from conception through the child’s fifth birthday. This amounts to $8,624 in additional costs to society for each mother-child pair annually.
The majority of maternal deaths are preventable. According to the CDC, 84 percent of pregnancy-related deaths are preventable (based on 2017-2019 data from 36 U.S. states). Mental health conditions, including deaths from suicide and overdose from substance use, are the leading cause of death during pregnancy and up to one year postpartum. Anxiety, perinatal and postpartum depression and birth-related post-traumatic stress disorder affect one in five women. Furthermore, 75 percent of women affected by mental health conditions one year postpartum do not receive treatment.
Homicide is also a leading cause of death for pregnant women in the U.S. pregnant and postpartum women are more likely to die from intimate partner violence (IPV) than the three leading obstetric causes of death, which include hypertensive disorders, hemorrhage or sepsis. In 2020, women who are pregnant or postpartum had a 35 percent higher risk of homicide compared with their peers, and 55 percent of victims were non-Hispanic, Black women. Non-Hispanic Black or African American individuals are more likely to experience adverse neonatal outcomes resulting from IPV and are more likely to be murdered during pregnancy or shortly after childbirth. Mental health and hemorrhages are now the leading causes of American Indian and Alaskan Native maternal deaths. Despite these poor outcomes, Maternal Mortality Review Committees found that between 2017 and 2019, 93 percent of pregnancy related deaths among American Indian and Alaskan Natives were preventable.
Underlying Causes Of America’s Maternal Health Crisis
Class, Culture, Sovereignty and Interpersonal and Institutional Discrimination
The direct and indirect effects of class, culture, sovereignty, interpersonal and institutional discrimination and poor social supports create compounding effects. Disparities occur across socioeconomic status, race, culture, age, geography, gender and disability status. The impacts of discrimination arise in the types of care available during pregnancy, the way care is delivered during childbirth and the systems and supports accessible to mothers, infants and families postpartum. Women who are Black, American Indian and Alaskan Native, rural or uninsured are at greater risk of experiencing these types of discrimination during the perinatal period.
As of the 2020 Census, American Indian and Alaskan Native population includes roughly 9.7 million people either identifying as American Indian and Alaskan Native alone or another racial group. Although this number represents just under three percent of the total U.S. population, it includes hundreds of distinct Tribal Nations with their own governments and cultures which requires a different set of approaches and solutions from states to address poor birth outcomes. Understanding the complex landscape of tribal jurisdiction is critical to unpacking the drivers behind these disparities in birth outcomes for American Indian and Alaskan Native outcomes. Further, tribal citizens are governed under layers of overlapping and adjacent government jurisdictions including state, federal and even country jurisdictions (for those bordering Mexico and Canada) which bifurcate the healthcare landscape. In December 2018, the U.S. Commission on Civil Rights’ Broken Promises report found that Tribal Nations face a decades-long funding crisis that is a direct result of chronic underfunding of Indian health care, which contributes to vast health disparities between American Indian and Alaskan Natives and other U.S. population groups.
Black persons are also burdened by disjointed systems of care for maternal health. Having a health care workforce that is representative of the community it serves is imperative to improving access to respectful care. As an example, as of 2021 there were fewer than 15 birth centers led by and serving people of color — out of more than 380 birth centers in the U.S. There are not enough supportive resources for and protections from intimate partner violence for mothers and infants, especially Black and American Indian and Alaskan Native women. Pregnant and new mothers, along with their babies, need better access to safe situations that secure their physical and mental health, employment and the well-being of their family.
The missing village. There has been a long-standing societal focus on babies, while mothers, their partners and others who make up the “village of child care” are often deprioritized in policy discussions. When a baby is born, millions of mothers do not have adequate paid time off to heal, care for their infant or bond as a family without jeopardizing their employment. Only 21 percent of U.S. workers have access to paid family leave through their employers. Further, there is not an accessible and affordable child care system to enable families to maintain steady employment and income. In 2021, one in three working families in the U.S. struggled to find needed child care. In the last five years, funding to increase access to childcare increased by 47 percent nationally. Further, there are no supports, universal education or health care services for fathers and partners in the perinatal health care system, yet one in ten fathers and adoptive parents experience postpartum depression, and they are often critical caregivers for both mothers and infants.
Insufficient coverage and a medical birth orientation. The approach to supporting pregnancy and childbirth in the U.S. has been clinically focused since the early 20th century, and there are few options for women and families to access culturally competent, community-based care. Peer countries to the U.S. have better maternal and infant health outcomes because their health care systems integrate community-based options for families, including access to doulas, lactation consultants and community health workers. Incorporating this expanded workforce into the maternal and infant system of care has also proven to lower costs.
Coverage for maternal health care has also been limited, though there have been recent efforts to expand coverage. In the U.S., perinatal care was established as an essential health benefit and required in health insurance coverage as recently as 2010. Extending Medicaid coverage beyond 60 days postpartum only began within the last two years, and even now this policy is only in select states. Additionally, Medicaid provided ten standard pediatric visits for infants within the first two years of life, but only provided mothers with one or two.
Leading institutes and associations are now calling for expanded coverage. The American College of Obstetricians and Gynecologists recently changed their guidance to call for more emphasis on the postpartum period, and Bright Futures, the guidance from the American Academy of Pediatrics, now includes maternal depression screening at four visits within the first year. Finally, despite the aforementioned evidence connecting maternal mortality and morbidity to mental health, there is no standard comprehensive mental health benefit integrated into federal Medicaid benefits and few maternal quality or equity measures.
ROADMAP LEXICON
Below are technical terms used frequently throughout the Roadmap.
Maternal mortality ratio: Death while pregnant or within 42 days of the end of pregnancy, irrespective of the duration and site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes. Used by the World Health Organization in international comparisons, this measure is reported as a ratio per 100,000 live births. When we examine historical trends, we use maternal mortality as our index.
Pregnancy-associated mortality: Death while pregnant or within one year of the end of the pregnancy, irrespective of cause. This is the starting point for analyses of maternal deaths.
Pregnancy-related mortality: Death during pregnancy or within one year of the end of pregnancy from: a pregnancy complication, a chain of events initiated by pregnancy or the aggravation of an unrelated condition by the physiologic effects of pregnancy. Used by the CDC to report U.S. trends, this measure is typically reported as a ratio per 100,000 live births. In this brief, when we discuss causes of maternal deaths and current rates, we generally use pregnancy-related mortality as our index.
Perinatal: Broadly, perinatal means occurring in, concerned with, or being in the period around the time of birth. The maternal and infant health field has more recently considered the time between conception through the first year postpartum as the perinatal period.
Perinatal Quality Collaboratives (PQCs): State or multistate networks of multidisciplinary teams, working to improve outcomes for maternal and infant health. There are currently 47 PQCs across the country that aim to advance evidence-informed clinical practices and processes using quality improvement principles to address gaps in care. PCQs work with clinical teams, experts and stakeholders, including patients and families, to spread best practices, reduce variation and optimize resources to improve perinatal care and outcomes.
Maternal Mortality Review Committees (MMRCs): Multidisciplinary committees that convene at the state or local level to comprehensively review deaths that occur during or within a year of pregnancy (pregnancy-associated deaths). They include representatives from public health, obstetrics and gynecology, maternal-fetal medicine, nursing, midwifery, forensic pathology, mental and behavioral health, patient advocacy groups and community-based organizations. The CDC works with MMRCs to improve review processes that inform recommendations for preventing future deaths and has funded MMRCs in 39 states and one U.S. territory.
At-risk populations: Women who live in the U.S. South, Midwest and rural counties or are Black and American Indian and Alaskan Native or uninsured face the greatest vulnerabilities to poor maternal health outcomes.
In The Face Of Crisis, Momentum On Reversing The Tide
U.S. states and territories have significant influence over women’s access to high-quality care during the perinatal period. Despite increased funding and attention toward the issue, rates of maternal and infant morbidity and mortality have seen minimal reductions, and inequities have, in some cases, increased. However, this is changing. Fueled by new data, increased focus from government leaders at the state and federal levels (see the 2022 White House Blueprint for Addressing the Maternal Health Crisis), growing media attention and thoughtful state-level planning, trends are starting to reverse.
At a national level, media attention and improved data and research are contributing to increased attention and guidance for states and territories. The March of Dimes Report Card, which reports on the condition of maternal and infant health across 53 states and territories, is released annually and serves as an important resource for states to identify the problems specific to key geographies and populations within individual states. National media outlets, such as the New York Times, are now frequently increasing mainstream attention to the issue.
States, including New Jersey and North Carolina, are developing state-level plans that engage diverse actors including state agencies, private philanthropy, community leaders and corporate partners in their design and execution. Private philanthropy is playing a critical role in facilitating connections across these actors by supporting infrastructure for collaboration, building databases (such as in California), investing in research and closing the divide between state government and community. See: Philanthropy’s Role in Advancing Maternal Health Equity: Collaborative Action and Funder Alignment for more detail on philanthropy’s role in advancing maternal health across states.
PHILANTHROPY’S ROLE IN ADVANCING MATERNAL HEALTH EQUITY: COLLABORATIVE ACTION AND FUNDER ALIGNMENT
Philanthropy plays a crucial role in partnering with state governments to address the urgent issue of maternal mortality and improve maternal health outcomes, particularly for marginalized communities. There are already several initiatives that showcase how collaborative action between philanthropy and state governments can achieve significant progress in policy design, awareness building, data systems improvement, policy implementation support and funder coordination.
Funding for Comprehensive State-Level Plan Design:
- The Perinatal Health Equity Collective in North Carolina, convened by the Department of Health and Human Services, developed the statewide Perinatal Health Strategic Plan, focusing on enhancing maternal and infant health.
- The Nicholson Foundation and the Community Health Acceleration Partnership (CHAP) funded in partnership with the Office of the New Jersey Governor Phil Murphy’s and First Lady Tammy Snyder Murphy’s offices, the creation of the Nurture New Jersey 2021 Strategic Plan which outlines goals for policy reform and provides actionable recommendations to improve maternal health outcomes.
Improving Data Systems:
- The California Health Care Foundation (CHCF) has worked on enhancing maternal health data systems to better understand and address health care disparities, including the publication of the Maternity Care in California report, which provides an overview of maternal care and health outcomes in the state.
- The California Maternal Quality Care Collaborative built a birth equity dashboard across partner hospitals, facilitating data-driven quality improvement initiatives.
Collaborative Policy Design and Implementation Processes:
- The National Academy for State Health Policy (NASHP), supported by philanthropic funds such as the Pritzker Children’s Initiative, provides resources and toolkits to help states improve maternal and infant health, including promoting Black maternal health and equity.
- The New Jersey Department of Health supported HealthConnect One to establish the New Jersey Doula Learning Collaborative, enhancing the number of trained community doulas and advocating for equitable compensation and reimbursement.vi Funders also supported the involvement of community doulas in the development of the state’s Medicaid reimbursement.
Supporting Narrative Change and Awareness Building:
- Every Mother Counts funded the film Giving Birth in America: Arkansas to raise awareness about the high maternal mortality rate in Arkansas.
- Narrative Nation’s podcast series Birthright, funded by CHCF and the Commonwealth Fund, amplifies positive birth stories of Black mothers and educates communities and health care providers.
Funding for Government Secondment Positions
- The New Jersey Birth Equity Funders Alliance is funding a two-year position for the director of the Nurture NJ effort, which will later transition into a permanent role within the Maternal and Health Innovation Center, an independent entity that works alongside state government and the first-of-its-kind maternal and infant health innovation center for excellence.
- Funders in North Carolina supported a philanthropy liaison position to build, strengthen and institutionalize relationships between state government and the philanthropic sector across a range of issues, including maternal and child health.
Funder Coordination and Alignment at the State and National Level
State-Level Alliances:
- The Birth Equity Catalyst Project (BECP), funded by CHAP, the Pritzker Children’s Initiative and Cambia Health, in partnership with Afton Bloom and Boldly Go, aims to address birth equity disparities through collaboration and collective action. Inspired by the New Jersey Birth Equity Funders Alliance, BECP aims to share effective models of philanthropic practice with other state funders looking to drive resources towards addressing inequities in birth outcomes.
National Funder Alignment:
- The Funders for Birth Justice and Equity is a national alliance of funders that works towards aligning and coordinating funders’ efforts to reduce racial disparities in birth outcomes.
- The inaugural Birth Equity Funders Summit (BEFS) in November 2022 brought together over 100 funders to reflect on philanthropy’s role and identify opportunities for collaboration and alignment, with a recently published BEFS report that outlines recommendations for philanthropy to advance birth justice and equity.
Priority 1: Build Infrastructure For Sustained Success
Maternal and infant health is a multifaceted issue that cuts across a vast array of domains in state government and stakeholder groups. State level planning, coordinated implementation and investment in infrastructure are necessary to drive concerted policy shifts. It is also critical to include lived experience voices and to center health equity in this work.
Most states have basic infrastructure in place to address maternal and infant health, such as a Maternal Mortality Review Committee (MMRC) and a state Perinatal Quality Collaborative (PQC), as well as a public health department or others that administer programs to target maternal and infant health issues. But few jurisdictions have articulated comprehensive strategies that are data informed and community inspired, identifying the unique needs within the state and laying out the full set of actions required to reverse disparities.
The collection, analysis and use of data is critical in ensuring continuous improvement and enhanced accountability. In states where there are many small, diverse populations, incomplete data practices can limit the insights into disparities and thus bar states’ ability to create solutions that meet the unique needs of different communities. For example, relatively small populations, like American Indian and Alaskan Native residents, are often overlooked, underfunded and left out of policy agendas, resulting in harm, despite having great health disparities. National reports and public data sets often fail to provide detailed information on American Indian and Alaskan Native people. Limited infrastructure to adequately support the relationships between state governments and leadership of sovereign Tribal Nations can also inhibit comprehensive solutions and resources that target specific groups. Further, creating and funding public awareness campaigns to reach families is another important role the state can play. This requires working with community leaders on tailored messaging to reach mothers and parents. Ensuring women’s voices are at the center of all this work is critical and will enable the development and funding of culturally competent programs.
OPPORTUNITY 1: DEVELOP A STATEWIDE MATERNAL HEALTH STRATEGIC PLAN AND ENSURE THAT BROAD REPRESENTATION IS AT ITS CENTER.
Governors can improve their state’s maternal health outcomes by creating and carrying out a comprehensive plan that engages multi-sector and community leaders in its design and execution. Many state departments and agencies intersect with and impact maternal and infant health, such as departments of health and human services, corrections, transportation and workforce development. It is helpful if a single agency or the Governor’s office champions the work and coordinates data sharing for holistic evaluations with relevant stakeholders, including community members and those directly impacted, to create a data-informed and community-inspired plan. Concerning community member outreach, a key step in developing a statewide strategic plan with broad representation may involve state governments convening with the Tribal Nation(s) in their state to identify the representatives to inform the plans and programs that aim to address maternal mortality and morbidity.
State Spotlight: The Michigan Department of Health and Human Services (MDHHS) launched its 2020-2023 Mother Infant Health & Equity Improvement Plan after “collaborating with communities to overcome barriers and build trust.” MDHHS is working alongside nine local and national maternal-infant health stakeholders to work toward zero health disparities, including Regional Perinatal Quality Collaboratives (RPQCs); Birth Detroit; Focus: HOPE; STRONG Beginnings; Michigan Maternal Mortality Surveillance (MMMS), Fetal Infant Mortality Review (FIMR); Women, Infants & Children (WIC); Michigan Alliance for Innovation in Maternal Health (MI AIM) and the Obstetrics Initiative (OBI). The New Jersey Nurture NJ plan, developed in partnership with 19 state departments and agencies and hundreds of partners including moms and families, outlines over 70 recommendations that target access to care, equitable systems of care and providing community environments that ensure women have the opportunity to be healthy. The North Carolina Department of Health and Human Services, with philanthropic partners, developed the statewide Perinatal Health Strategic Plan, focusing on enhancing maternal and infant health. The Attorney General’s office in the State of Washington established a new state policy that requires Tribal consent and consultation prior to the initiation of a program or project that directly and tangibly affects Tribes, Tribal rights, Tribal lands and sacred sites.
Opportunity 2: DEVELOP A PROPOSAL FOR A STATE MATERNAL HEALTH INNOVATION (MHI) PROGRAM THROUGH THE FEDERAL HEALTH RESOURCES & SERVICES ADMINISTRATION (HRSA) TO SUPPORT STATE PLANNING AND INFRASTRUCTURE.
The purpose of the State Maternal Health Innovation (MHI) program is to support state-led demonstrations focused on improving maternal health through quality services, a skilled workforce, enhanced data quality and capacity and innovative programming. This program also engages public health professionals, providers, payors and consumers through state-led Maternal Health Task Forces. These task forces review state-specific maternal health data and implement evidence-based interventions and innovations that address critical gaps.54F[i]
State Spotlight: Two cohorts of nine states each received MHI grants for a five-year period. Iowa was awarded a grant in 2019 to develop an Iowa Maternal Quality Care Collaborative. The Collaborative aimed to improve state-level maternal health data and surveillance, implement initiatives to address workforce shortages for obstetrical care, expand existing telemedicine initiatives to increase access to maternal-fetal medicine specialists and mental health professionals, and address health disparities in maternal health outcomes and access to care.55F[ii]
Opportunity 3: EXPAND FUNDING FOR THE STATE MATERNAL MORTALITY REVIEW COMMITTEE TO IMPROVE MATERNAL HEALTH DATA COLLECTION AND SHARING TO REDUCE PREVENTABLE PREGNANCY-RELATED DEATHS.
Maternal Mortality Review Committees (MMRCs) identify medical and social factors that contribute to maternal deaths and inform priorities for states to better prevent maternal mortality. In the past, MMRCs have identified complications such as maternal depression, the need for safe transport, specific risk disparities for those experiencing domestic violence, cardiovascular disease, hypertension and hemorrhage as significant risk factors. Two best practices include (1) standardizing data collection between states to ensure that no maternal death is missed and (2) including community perspectives to have a more comprehensive understanding of the factors contributing to maternal deaths. The inputs and findings elevated by the MMRCs should inform the state-level goals and strategies, specifically informing perinatal quality collaboratives regarding which health areas can be improved.57F[ii] Finally, there is a specific need to mobilize state agencies alongside Tribal Nation representatives to improve racial and ethnic data to accurately represent American Indian and Alaskan Native people, including oversampling of American Indian and Alaskan Native persons to address small sample size concerns.
State Spotlight: Thirty-nine states have obtained funding from the CDC through the Enhancing Reviews and Surveillance to Eliminate Maternal Mortality (ERASE MM) Program to improve data collection on maternal morbidities in their states. Through these mechanisms, policymakers can identify maternal and infant health risks and recommend data-informed policies to address these needs. For example, the Mississippi Department of Health recommends that preconception counseling is available to women with high mortality medical conditions and that state agencies provide information on location and operating hours of emergency care in rural areas. The Maternal, Child and Adolescent Health Section in Nevada recommends educating providers on Nevada’s substance use disorder treatment options, which already exist for pregnant women, and removing barriers to care. The Maternal Mortality Review Committees in Texas and Oklahoma have added seats to include people with lived experience to identity gaps in maternal healthcare. Ohio implemented a data-sharing arrangement between the Department of Health and Department of Administrative Services to link longitudinal data on maternal engagement with state systems in support of identifying health risks while expanding and evaluating the home visiting program for at-risk mothers. States may also include Tribal Epidemiology Centers, which are also legally recognized Public Health Authorities, in MMRCs to promote better data quality, collection, collaboration and security.
OPPORTUNITY 4: IDENTIFY REGIONAL VARIATIONS IN MATERNAL HEALTH.
A landscape analysis of the maternal and infant health variations can identify the communities that are most susceptible to maternal health disparities and better inform interventions. Under the federal Data Mapping to Save Moms’ Lives Act, states should soon have access to maps from the Federal Communications Commission that overlay broadband access with maternal health data.
State Spotlight: The New York State Department of Health analyzes 18 maternal and infant health outcomes such as infant mortality, preterm birth and low birthweight to determine maternal and infant health hot spots across the state.
OPPORTUNITY 5: ESTABLISH A DATA ENTITY THAT PRODUCES STATEWIDE DATA ON MATERNAL HEALTH OUTCOMES AND PARTNERS WITH HOSPITALS TO IMPLEMENT BETTER PRACTICES.
Data can inform states on the scope of disparities in maternal and infant health outcomes. There are commonly used population-based information sources that may have maternal and infant data, but data utility can significantly improve under an established entity tasked with and committed to implementing better collection and evaluation practices. It is also important to rely on existing and available data where possible to avoid further burdening people with lived experiences by relying solely on their voices to demonstrate maternal and infant health disparities.
State Spotlight: Since 2006, the California Maternal Quality Care Collaborative (CMQCC) has worked to improve maternal outcomes by gathering data on maternal mortality and analyzing maternal morbidities and disparities through the CMQCC Maternal Data Center. CMQCC has produced four publications on quality improvement measures for the state of California and authored more than 70 research publications on maternal health.
Priority 2: Increase Access To Perinatal Care
A 2020 report by the Centers for Medicare & Medicaid Services (CMS) notes that in an ideal maternal health system, all people would have access to comprehensive, seamless medical and behavioral health care as well as economic and social supports. Additionally, they would be engaged with this system before, during and after pregnancy, and care would be available in places more proximate than a hospital. The majority of women in the U.S. do not receive this type of care.
For most Americans, access to health care starts with health insurance. Health care coverage before and after pregnancy is associated with better health outcomes for both mother and infant. One example is coverage for prenatal care. Babies of mothers who do not get prenatal care are three times more likely to have a low birth weight and five times more likely to die than those born to mothers who do get care. With the implementation of the Affordable Care Act (ACA), health insurance coverage expanded dramatically for most citizens of the U.S. However, there is more that states can do to ensure that prenatal, delivery and postpartum care are available to women through a comprehensive insurance coverage plan.
Health insurance coverage should include support for perinatal mental health and substance use disorders, from screening through treatment, to address the leading causes of maternal mortality. Coverage could also include postpartum care that extends beyond the traditional single visit six weeks postpartum. Slightly more than half (52 percent) of all deaths occur after the day of delivery through one year postpartum, while almost one-third (31 percent) occur during pregnancy.
Ultimately, it is critically important for both commercial and public health insurance to include robust perinatal coverage, especially behavioral health services and longer-term postpartum care. The ACA greatly improved coverage of maternity health services. In particular, 20 million people have gained coverage, financial assistance has become available to purchase coverage and the quality of coverage offered has been improved. But there are still significant differences among states in the prenatal, labor and delivery, and postpartum services covered. Specifically, the ACA requires small group and individual market plans to cover maternity and newborn care among the required essential health benefits (EHBs), but states are able to select a benchmark plan to define the specific services covered under each category which can serve to limit coverage. Similarly, there is a great deal of variation in services and outcomes offered through Medicaid. In 2021, 41 percent of births in the U.S. were financed by Medicaid. However, compared to women with private health insurance, women with Medicaid coverage were more likely to report: no postpartum visit, returning to work within two months of birth, less postpartum emotional and practical support at home, lack of decision autonomy during labor and delivery, being unfairly treated and disrespected by providers because of their insurance status and not exclusively breastfeeding at one week and six months.
Opportunity 6: EXPAND MEDICAID TO 365 DAYS POSTPARTUM.
Extending Medicaid coverage through 12 months postpartum is crucial to addressing the current maternal health crisis. The first year after birth is a significant period, as more than half of pregnancy-related deaths happen during this time. Extending coverage can help new mothers overcome barriers to physical and mental health care, improve health outcomes and potentially reduce disparities. Approximately 65 percent of births by Black mothers are covered by Medicaid, so extending the postpartum coverage would positively impact outcomes and reduce disparities.
Currently, the default for Medicaid coverage ends 60 days after birth, but through Section 9812 of the 2021 American Rescue Plan Act states have the option of extending Medicaid 12 months postpartum through a less cumbersome administrative processes, as well as drawing on more federal matching funds.79F[iii] The American College of Gynecology guidance notes that the postpartum period should be an ongoing process “with services and support tailored to each woman’s individual needs.” This may include physical recovery from birth, an assessment of social and psychological well-being, chronic disease management and initiation of contraception, among other services. Under the Consolidated Appropriations Act of 2023, the extension option for Medicaid postpartum coverage has been made permanent. Therefore, once states choose to extend, they will continue to receive federal matching funds.
State Spotlight: As of June 2023, 35 states have extended their postpartum coverage through a full year postpartum. Louisiana was a national leader in extending postpartum coverage. The Centers for Medicare Services approved the state’s plan amendment in April 2022. States have approached this through combinations of federal action, state plan amendments or waivers, and laws or bills.
Opportunity 7: EXPAND EVIDENCE-BASED HOME VISITING PROGRAMS.
Home visiting is a prevention strategy designed to support pregnant families, promote infant and child health, foster child development and school readiness, and help prevent child abuse and neglect. Home visiting programs are voluntary and offer vital support to parents as they manage the challenges of raising babies and young children.
States are covering these evidence-based services, such as home visiting during the perinatal period, to improve continuity of care for pregnant and postpartum people enrolled in the Medicaid Children’s Health Insurance Program (CHIP). States leverage other federal, state, local and private funding sources to finance these services and in some cases use existing Medicaid services to cover components of home visiting.
One example of a robust universal home visiting model is Family Connects, which is part of a clearinghouse of highly effective approaches. Family Connects demonstrates improvements in child health, linkages and referrals, maternal health and positive parenting practices. It consists of one to three nurse home visits, typically when the infant is two to 12 weeks old, and follow-up contacts with families and community agencies to confirm families’ successful linkages with community resources. During the initial home visit, a nurse conducts a physical health assessment of the mother and newborn, screens families for potential risk factors and may offer direct assistance, such as guidance on infant feeding and sleeping. If a family has a significant risk or need, the nurse connects the family to community resources. Family Connects is currently implemented in 12 states.
State Spotlight: In 2019, Kansas served an estimated 23.8 percent of children under age three in families with incomes of less than 150 percent of the Federal Poverty Level in the state’s home visiting programs. As of 2021, families in the state have access to five out of a possible seven evidence-based program models that have a demonstrated impact on parenting and are designed for families with young children. In 2021, Maryland launched a maternal and child health care transformation initiative to fund the expansion of current maternal health-focused programs, which includes home visiting services. In Michigan, the statewide Maternal Infant Health Program serves over 20,000 Medicaid-eligible families, with prenatal and postnatal home visiting covered. Michigan is creating more awareness of their Home Visiting Program and other state maternal health programs by developing a mobile pregnancy app to connect users to state maternal health programs. In 2021, New Jersey joined Oregon in enacting Universal Newborn Nurse Home Visiting enabling all new moms, including those that experience a stillbirth and those that adopt, to receive up to three visits by a registered nurse in their home. Additional states with robust home visiting programs include Iowa and Maine.
Opportunity 8: PROVIDE PRESUMPTIVE ELIGIBILITY TO ALLOW PROVIDERS TO TREAT PREGNANT PEOPLE WHEN THEY FIRST SEEK PRENATAL CARE RATHER THAN WAITING UNTIL AFTER MEDICAID ELIGIBILITY IS REVIEWED AND DETERMINED.
Despite being eligible for Medicaid coverage, it often takes pregnant women days or sometimes weeks to acquire Medicaid, delaying their prenatal care and treatment. Presumptive eligibility is a policy that allows health care providers to provide temporary Medicaid or CHIP coverage to individuals who are likely to qualify for these programs but have not yet completed the application process.
State Spotlight: As of 2020, 30 states, offer presumptive eligibility for pregnant women. Express Lane Eligibility (ELE) is another policy that could increase access to Medicaid services for eligible women while also streamlining the application process. ELE allows state Medicaid or CHIP programs to rely on the application findings from other state programs, such as Head Start or the Supplemental Nutrition Assistance Program (SNAP), to offer health care services. As of 2021, ELE is offered in Alabama, Colorado, Iowa, Louisiana, Massachusetts, South Carolina and South Dakota.
Opportunity 9: EXPAND ACCESS TO MATERNAL AND INFANT CARE FOR UNINSURED POPULATIONS.
Lawfully present immigrants may qualify for Medicaid and CHIP but are subject to certain eligibility restrictions. In general, lawfully present immigrants, including most lawful permanent residents or green-card holders, must have a “qualified” immigration status to be eligible for Medicaid or CHIP and must wait five years after obtaining qualified status before they may enroll. Noncitizens, including lawfully present and undocumented immigrants, are significantly more likely to be uninsured than citizens. Medicaid expansion to households with 200 percent of the federal poverty level, allowing Deferred Action for Childhood Arrivals (DACA) eligible immigrants to receive CHIP prenatal services and reducing the five-year Medicaid eligibility waiting period for immigrants can cover these gaps in care during the perinatal period.
State Spotlight: In 2021, Oregon implemented the Cover All People legislation as part of House Bill 3352 to include low-income, undocumented adults in the Oregon Health Plan. As of July 2022, there is $100 million in state funding for the expansion. In July 2022, Illinois lowered the age for Medicaid eligibility for residents regardless of citizenship to 42 years old through authorization from the Illinois General Assembly.
Opportunity 10: FUND AND PRIORITIZE INTEGRATED SCREENING, REFERRALS AND CARE FOR PERINATAL MOOD AND ANXIETY DISORDERS (PMADS), PERINATAL SUBSTANCE USE DISORDERS (SUDS) AND INTIMATE PARTNER VIOLENCE (IPV).
As the most common complications in pregnancy, PMADs, SUDs and IPV are distinct yet often intertwined, and associated with a range of adverse outcomes for pregnant persons and their families. Some estimates indicate that 15.9 percent of pregnant people in the United States smoked cigarettes, while 8.5 percent consumed alcohol and 5.9 percent used illicit drugs. IPV can result in insufficient or inconsistent prenatal care, poor nutrition, inadequate weight gain, substance use and increased prevalence of depression, as well as adverse neonatal outcomes, such as low birth weight and preterm birth and maternal and neonatal death.
Routine screenings, interventions and referrals through an integrated care model for mothers and their families are essential. Markers of strong, integrated care include: training health care providers to identify mental health, substance use and IPV issues for pregnant and postpartum women, early and periodic screening that supports both identification and stigma reduction through frequent conversations with families, accessing treatment across the continuum of mild to severe issues, and working with pediatric providers to screen and support mothers and families with mental health and substance use disorders throughout the first year of well-child visits.
State Spotlight: Alabama expanded Medicaid to include screening, brief intervention and referral to treatment for early intervention and treatment of SUDs. In 2021, Louisiana began allowing separate Medicaid reimbursement for perinatal depression screenings of an enrolled caregiver during a well-child visit from birth to 365 days postpartum. In New Mexico, pregnant women of color reported receiving discriminatory substance use treatment and screening, so the New Mexico Children, Youth and Families Department (CYFD) and the Department of Health (DOH) created systemic training for hospital staff to provide less stigmatizing treatment. Further, the Children’s Code was amended through House Bill 230 so that substance use during pregnancy is not singular grounds for a mandatory child abuse report. New Mexico’s amendment to the Children’s Code included a Plan of Safe Care in which families affected by substance use make a plan during pregnancy with a multidisciplinary team to ensure the health of infants and mothers. Plans of Safe Care include the following four components for care and support during the perinatal period: physical health, behavioral health to address substance use, infant health and development and parenting/family support to connect the family with social services. Currently, 33 states have Plans of Safe Care to address the needs of infants and mothers.
Opportunity 11: PROVIDE MEDICAID REIMBURSEMENT FOR MORE TELEHEALTH MODALITIES, INCLUDING LIVE VIDEO, STORE-AND-FORWARD, REMOTE PATIENT MONITORING, TELE-ULTRASOUND, REMOTE NONSTRESS TEST AND EMAIL/PHONE/FAX.
With the national increase in maternal care deserts, people across the country are being forced to travel further for perinatal care. Adoption of Medicaid reimbursement policies and ensuring that codes for these procedures allow, or even specify, that the activity can take place in the home is important because it allows patients to be monitored and cared for without the cost and burden of frequent prenatal visits.
Two U.S.-based studies investigated a combination of telehealth visits and reduced in-person visits for prenatal care to determine the feasibility of telehealth maternal care. The two studies demonstrated that telehealth resulted in higher satisfaction and lower prenatal stress for patients compared with those receiving in-person care. It is necessary to note that telehealth can only be effective if access to technology is universal.
State Spotlight: The Extension for Community Healthcare Outcomes, Project ECHO, is a tele- mentoring approach that brings expertise to patients in medically underserved areas by connecting specialty physicians to primary care physicians. Project ECHO, which began in New Mexico, is now one of the many maternal telehealth policies in Virginia aimed at improving health coverage and supporting the alignment of reimbursement for telehealth services across patients. In Georgia, the Healthy Babies Act was passed in 2023 to pilot a two-year maternal telehealth program for Medicaid enrollees that provides access to remote patient monitoring, remote fetal nonstress tests and tele-ultrasound. In Missouri, the Medicaid Department issued guidance clarifying that the home can be a place of service for the fetal non-stress test. In Oklahoma, expanding telehealth services for birthing women and infants is part of the Oklahoma Maternal Health Task Force 2020-2024 Strategy.
Opportunity 12: FUND THE STATE’S PERINATAL QUALITY COLLABORATIVE (PQC) TO INCREASE CAPACITY AND SUPPORT PAY-FOR-PERFORMANCE MODELS.
Nearly every state already has or is developing a PQC, which supports hospitals and clinicians to engage with quality improvement tools. PQCs have made population health improvements by improving breastfeeding rates, reducing elective deliveries without a medical indication before 39 weeks’ gestation, reducing unnecessary cesarean births among low-risk pregnant women, reducing health care setting-associated infections in newborns, bringing down rates of hemorrhage and hypertension and reducing rates of preterm births.
About half of states monitor or report state-level metrics related to maternal health. While most states require managed care organizations to report maternity-related quality measures to the state, few use performance improvement measures. Quality improvement tools may be more widely used by incorporating pay-for-performance models or by adopting existing perinatal risk assessment tools. There is a need to invest more resources into PQCs and provide capacity support to expand the impact of their work.
State Spotlight: To address rising maternal deaths associated with preeclampsia, Illinois’ PQC conducted a program to improve care for pregnant and postpartum women with severe preeclampsia and eclampsia in 112 hospitals. The number of women receiving medication within 60 minutes increased from 42 percent to 85 percent during the program, and the rate of severe pregnancy complications among pregnant women experiencing hypertension at delivery decreased by 41 percent.
Opportunity 13: ENSURE ACCESS TO COMPREHENSIVE EVIDENCE-BASED CHILDBIRTH EDUCATION FOR ALL MEDICAID BENEFICIARIES AS PART OF STANDARD PRENATAL CARE.
Childbirth education (CBE) is designed to help pregnant women and their support unit manage the physical, emotional and psychological changes during the perinatal period, increase their knowledge and access to community resources, improve their ability to advocate for care and increase the likelihood of positive birth outcomes. CBE is also a recommended strategy for cesarean rate reduction.
States can work with their perinatal quality collaborative to align hospital practices and philosophies with evidence-based childbirth education; assess and mitigate barriers to childbirth education; include flexible educational formats, such as interactive web-based learning; and implement prenatal care models that efficiently integrate comprehensive pregnancy and childbirth education into routine visits, such as group prenatal care.
State Spotlight: Washington’s Medicaid program offers pregnant women a series of educational group sessions with at least six hours of instruction, led by a trained educator who has both a certification or credentials from a training organization that meets the Childbirth Educator training standards set by the International Childbirth Education Association (ICEA) and a current Core Provider Agreement and National Provider Identifier (NPI), to prepare each pregnant woman and her support person(s) for labor and delivery. In Wisconsin, CBE is covered through Medicaid if a pregnant person is both at higher risk for adverse outcomes and are also enrolled in the state’s Prenatal Care Coordination program.
Opportunity 14: IMPLEMENT PRENATAL AND POSTPARTUM PATIENT SAFETY BUNDLES TO ADDRESS ONGOING QUALITY IMPROVEMENT.
Patient safety bundles are a structured way of improving the processes of patient care.108F[i] The Alliance for Innovation on Maternal Health (AIM) is a quality improvement initiative to support best practices that make birth safer, improve maternal health outcomes and save lives by implementing best practices in hospitals. AIM developed eight bundles that include actionable steps that can be adapted to a variety of facilities and resource levels to address the leading causes of preventable maternal mortality.
State Spotlight: In Texas, the Department of State Health Services (DSHS) teamed up with AIM and the Texas Hospital Association to create the TexasAIM initiative to help hospitals and clinics carry out maternal safety projects. Currently, TexasAIM supports three AIM bundles such as the Obstetric Hemorrhage Bundle, the Obstetric Care for Women with Opioid Use Disorder Bundle and the Severe Hypertension in Pregnancy Bundle. The Texas DSHS connects any interested hospitals and clinics to resources, tools and the AIM data portal.
Opportunity 15: HOLD PROVIDERS ACCOUNTABLE FOR ENSURING THAT A RECENT PREGNANCY OR BIRTH IS INCLUDED AS PART OF THE STANDARD PATIENT INTAKE PROCESS.
Maternal and infant health outcome improvement is challenged by the number of fragmented touchpoints in a health care system that exist from conception through one year postpartum. For example, a woman may shift from a midwife-led clinic to a hospital delivery with an OB-GYN provider, then go back to a primary care provider in the postpartum period, followed by another shift to having the majority of interactions with their child’s pediatrician. Encouraging connection and communication among this system of providers is another approach to ensuring accountability for high-quality care and outcomes.
State Spotlight: In 2020, New Jersey enacted bill A5031/S3455, which requires hospital emergency departments to ask people of childbearing age about any pregnancy in the past 365 days. This simple approach could lead to catching health issues exacerbated by a pregnancy-related condition a full year postpartum.
Priority 3: Focus On Disparities Affecting Black And American Indian And Alaskan Native Persons
Stark racial disparities in maternal and infant health in the U.S. have persisted for decades despite continued advancements in medical care. It is not enough to focus on addressing gaps within the formal health care system without specifically, deliberately and inclusively putting resources toward the factors that contribute to these disparities. Notably, disparities in maternal and infant health persist even when controlling for certain underlying social and economic factors, such as education and income, pointing to the roles that interpersonal and institutional discrimination play in driving disparities.
The Kaiser Family Foundation highlights research documenting that social and economic factors, racism and chronic stress contribute to poor maternal and infant health outcomes, including higher rates of perinatal depression and preterm birth among Black and American Indian and Alaskan Native women and higher rates of mortality among Black infants. In one study, American Indian and Alaskan Native, Hispanic and Black women reported significantly higher rates of mistreatment, such as shouting and scolding or ignoring or refusing requests for help, during the course of their pregnancy. Even controlling for insurance status, income, age and severity of conditions, Black, American Indian and Alaskan Native and Hispanic people are more likely to experience a lower quality of care and less likely to receive routine medical procedures.
Governors and policy leaders can increase awareness of interpersonal and institutional discrimination and unintended biases through mechanisms like implicit bias training for all individuals that have touchpoints with mothers and children. One way to improve health outcomes and government efficiency is to break down silos across agencies, public and private institutions and providers — especially in sectors that may seem unrelated at first glance, like corrections — and to integrate care models and supports with an awareness of racism and how communities can and should lead on solutions to provide equitable care.
Opportunity 16: CENTER EQUITY IN ANY MATERNAL HEALTH INITIATIVE.
In addition to creating an equitable statewide maternal health plan, any maternal health-related initiative or policy should center equity, whether it has a clinical or community focus. States and hospital networks have centered equity in their health policies as a way to build trust and achieve optimal health for all patients. The American Medical Association offers a toolkit with five steps to embed equity into health systems to achieve optimal health for each patient.
State Spotlight: In Ohio, the Eliminating Racial Disparities in Infant Mortality Task Force published recommendations to improve maternal health as well. In Washington, University of Washington Medicine launched the Healthcare Equity Blueprint for 2022-2026 with key areas for clinical improvement to better meet the needs of marginalized communities.
Opportunity 17: PROMOTE AND PROVIDE ACCESS TO CULTURAL HUMILITY AND IMPLICIT BIAS TRAINING FOR EVERYONE IN THE MATERNAL CARE CONTINUUM.
The American Journal of Public Health published a systematic review that examined the degree to which implicit bias toward race and ethnicity exists in health care professionals and how the bias changes health care outcomes. The results revealed a significant relationship between implicit bias and four areas of patient care: patient–provider interactions, treatment decisions, treatment adherence and patient health outcomes. Implicit bias is more likely to occur in stressful situations when health care professionals are tired, busy and feeling pressured.
State Spotlight: As of 2023, the Michigan Department of Licensing and Regulatory Affairs includes guidelines requiring nursing professionals seeking licensure or registration to complete a one-hour implicit bias course from a board-approved continuing education provider to meet this requirement within their first two years after licensure. Implicit bias training is also now incorporated into nursing training education. In 2021, New Jersey enacted a law requiring all health care professionals who provide perinatal treatment and care at a hospital or birthing center undergo explicit and implicit bias training. In North Dakota, a 20-minute implicit bias training is available on the state’s Health and Human Services website intended for professionals in healthcare, education and social services.
Opportunity 18: DEVELOP PUBLIC-PRIVATE PARTNERSHIPS TO IMPLEMENT PLACE-BASED, COMMUNITY-PARTNERED CHANGE MODELS IN AREAS WITH THE HIGHEST MATERNAL AND INFANT MORBIDITY AND MORTALITY, AND THEN EXPAND TO EVERY COMMUNITY ACROSS THE STATE.
Closing the gap between maternal and infant health disparities and reducing mortality requires engagement from stakeholders at all levels, including buy-in from the communities most impacted by these outcomes. Partnering with philanthropic groups can provide a neutral space to connect with stakeholders outside of government and support the identification of the right partners and priorities to highlight as part of this work.
State Spotlight: The Safer Childbirth Cities initiative is a nationwide effort to engage private and public stakeholders to foster local solutions and implement community-partnered change to reduce the racial inequities in maternal health outcomes. Currently, 20 cities participate in the initiative to implement strategies tailored to the needs of pregnant people in their city. A few of these strategies include community-partnered change such as incorporating integrative care, connecting women to clinics and providing doula support. In New Jersey, the Maternal Experience Survey is a community tool developed by the Atlantic City NAACP Black Infant and Maternal Mortality (BIMM) task force to improve care and reduce childbirth-related disparities for women of color. The task force is composed of health professionals, legislators, educators and community members and is responsible for building community-level action to improve the birthing outcomes for people in New Jersey. The Inter-Tribal Council of Arizona, Inc. created the Maternal Health Innovation Program and strategic plan to improve maternal health outcomes in Tribal communities. The comprehensive plan identifies seven priority areas alongside specific action items to meet their goals to improve maternal mortality and morbidity in Tribal communities in Arizona, improve access to maternal health surveillance data, and improve the maternal health partnership between Tribal communities and Arizona.
Opportunity 19: SUPPORT A STATEWIDE CAMPAIGN TO RAISE AWARENESS OF STATISTICS, RESOURCES AND LIFE-THREATENING SIGNS DURING AND AFTER PREGNANCY.
The Hear Her Campaigns are CDC public awareness campaigns to raise awareness of potentially life-threatening warning signs during and in the year after pregnancy. They encourage the people supporting pregnant and postpartum women to listen and act when concerns are expressed. Hear Her began in 2019 as a national campaign to reach Black Americans, American Indians and pregnant women and their partners in addition to healthcare providers. Community-based organizations, hospitals and many states have adopted the framework and adapted it for their state contexts.
State Spotlight: The Texas Department of Health and Human Services adapted the Hear Her Campaign to produce video PSAs, information on early warning signs and risks and stories from pregnant women. All resources are available in English and Spanish. The Arizona Department of Health and Human Services is launching a Hear Her Campaign with the following goals: increase awareness of serious pregnancy-related complications and their warning signs, empower women to speak up and raise concerns, encourage women’s support systems to have conversations with her about symptoms, and provide tools to facilitate these conversations for women and providers. In 2022, the CDC Foundation partnered with the Health and Human Services Office of Minority Health to highlight the stories of five pregnant American Indian and Alaskan Native women through the Hear Her Campaign and adapted the urgent warning signs resources to be culturally appropriate, including resources for healthcare professionals who work with American Indian and Alaskan Native populations. While the American Indian and Alaskan Native Hear Her Campaign is nationwide, Montana Obstetrics and Maternal Support includes the campaign as part of statewide maternal health resources.
Opportunity 20: IMPROVE MATERNAL HEALTH CARE FOR WOMEN WHO ARE INCARCERATED.
Up to 75 percent of women who are incarcerated are of childbearing age, and Black women are impacted at twice the rate of white women. The available estimates for the rate of pregnancy for women who are incarcerated is between three to four percent at intake. Often, incarceration is linked to higher pregnancy risk factors such as substance use, poverty and mental health conditions. Some prisons are beginning to offer perinatal support such as parenting programs, nurseries, and midwifery and doula care.
State Spotlight: In Pennsylvania, commonwealth health and corrections departments partnered with the Tuttleman Foundation and Genesis Birth Services to launch a pilot doula program for incarcerated pregnant people. The state has allocated $100,000 of American Rescue Plan Act funding as well. As part of the program, incarcerated expecting mothers have access to prenatal visits, biweekly checkups and doula support during births. The program is now expanding to include a lactation program that will allow incarcerated mothers to pump and mail milk to their babies. The 2021, Colorado Birth Equity Bill Package includes the protection of all pregnant people in their perinatal period, including incarcerated women. Protections include requirements for correctional facilities, jails and prisons to report the use of restraints on pregnant women. Similarly, Illinois has extensive laws to protect incarcerated women during the perinatal period including their right to not be shackled during birth, right to be without a correctional officer present during birth, choice in cesarean birth or epidural, right to refuse induced labor, and right to be screened for the Moms and Babies program in addition to accessing education on childbirth and pregnancy.
Opportunity 21: ENSURE THAT STATE LAWS INCREASE BREASTFEEDING INITIATION AND CONTINUATION RATES, DECREASE DISPARITIES AMONG BREASTFEEDING MOTHERS AND PROVIDE BREASTFEEDING SUPPORT FOR MOTHERS, FATHERS AND OTHER PARTNERS.
Mothers and children benefit from breast milk. Exclusively breastfed infants tend to need fewer health care visits, prescriptions and hospitalizations, resulting in a lower total medical care costs compared with never-breastfed infants. Breastfeeding also provides long-term preventive effects for the mother, such as a reduced risk of pre-menopausal breast cancer and osteoporosis.134F[ii] Although rates of breastfeeding initiation have increased during the past decade, racial and ethnic disparities in breastfeeding persist.
Federally, in 2019, Congress passed the Fairness for Breastfeeding Mothers Act, which requires certain public buildings to provide a shielded, hygienic space other than a bathroom for members of the public to express milk. There are also many state-level policy options to support breastfeeding and assess the impact.
State Spotlight: In Maryland, child care centers are required to promote proper nutrition by establishing training to promote breastfeeding in accordance with the 2014 Education Code 9.5 404. In New York, the Breastfeeding Mothers’ Bill of Rights must be posted in maternal health care facilities, and the state allows a child under one year of age to accompany the mother to a correctional facility if the mother is breastfeeding at the time she is committed. New Jersey requires lactation rooms in certain healthcare and government buildings, including the state capital building, exempts breast pump supplies and repairs from state sales and use taxes, and requires Medicaid to cover human donor milk under certain circumstances. The following states require health insurance plans to provide coverage for assistance and training in breastfeeding: Massachusetts, Minnesota, Missouri, Nevada, New Jersey, New York, Ohio, Oklahoma, Oregon, Pennsylvania, Rhode Island and Texas.
Priority 4: Focus On Nonmedical Root Causes
Over the last two decades, and apart from medical care, a large and compelling body of evidence has elevated the powerful role of social factors in shaping health across a wide range of indicators, settings and populations. Using an ecological model of perinatal health demonstrates the complexity and need to address the major drivers of perinatal health at each level of the social-ecological model.
The Maternal Vulnerability Index (MVI) by Surgo Ventures is a useful open-source tool that examines a range of factors nationally that influence adverse pregnancy outcomes, including both structural and individual level-factors, and identifies precisely where and why mothers are more vulnerable to maternal mortality. This tool ranks counties and states on overall vulnerability to poor pregnancy outcomes and six related themes:
- Reproductive health care: access to and availability of family planning and perinatal care
- Physical health: prevalence of noncommunicable diseases and sexually transmitted infections
- Mental health & substance use: mental health status, access to mental health care and prevalence of substance use issues
- General health care: health system accessibility, affordability and quality
- Socioeconomic determinants: educational attainment, poverty and food insecurity
- Physical environment: lack of access to transportation, severe housing problems, violent crime and pollution
One of the findings of the MVI is that Black and American Indian and Alaskan Native women of reproductive age are more likely to live under conditions that are not conducive to good maternal health ,a sign of structural factors linked to racial health disparities. Women in the South face the greatest maternal vulnerability of the four regions in the U.S.; they are more than twice as vulnerable than women in the Northeast and West. However, the largest gaps between white and Black maternal health outcomes exist in the Midwest where divergence is driven by differences in socioeconomic determinants, physical environment and physical health status.
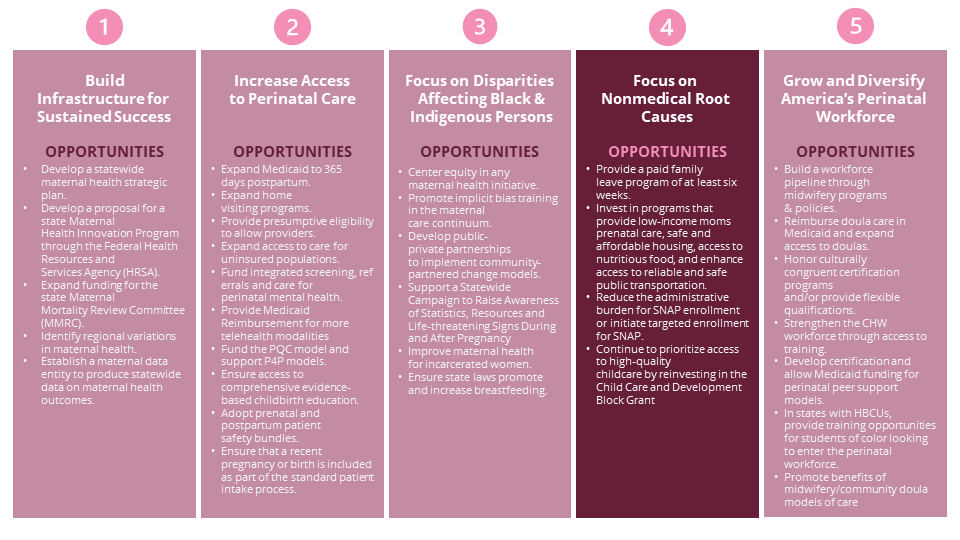
Opportunity 22: PROVIDE A PAID FAMILY LEAVE PROGRAM OF AT LEAST SIX WEEKS.
State paid family leave programs require employers to allow eligible parents time off from work to bond with a new child while receiving a portion of their wages. These programs allow parents to stay home with their infant while ensuring their economic security and keeping them in the workforce. They also enable parents to bond with their infant and develop caregiving skills, seek timely treatment for themselves and the child, and develop a healthy infant-parent attachment.
Paid family leave policies govern how much paid time off employers must provide to an employee after birth, adoption or placement of a foster child. According to the Bureau of Labor Statistics, as of March 2021, 23 percent of all workers had access to paid family leave, and 89 percent of workers had access to unpaid family leave. A minority of states have adopted paid family leave policies, so for many workers, access to paid family leave is dependent on the generosity of employer-offered benefits. Access to paid leave remains highly skewed toward adults with higher incomes, with college degrees and with full-time jobs.
State Spotlight: California, Connecticut, Maine, New Jersey, New York, Rhode Island and Washington have paid family leave of at least six weeks. Since 2022, Connecticut families receive 12 weeks of paid family leave. By 2026, Delaware, Maryland and Oregon will have fully implemented 12-week paid family leave programs.
Opportunity 23: INVEST IN PROGRAMS THAT PROVIDE MOMS WITH LOW-INCOME PRENATAL CARE, SAFE AND AFFORDABLE HOUSING AND ACCESS TO NUTRITIOUS FOOD, AND ENHANCE ACCESS TO RELIABLE AND SAFE PUBLIC TRANSPORTATION.
Differences in the availability of resources driven by systemic factors have led to pronounced inequities in access to quality health care and education, food security, safe housing and employment, ultimately producing racial disparities in health outcomes. For example, hypertension and lack of physical activity are pre-pregnancy conditions that are influenced by the availability of safe places to exercise and access to affordable, nutritious food. Investment in programs that overcome disparities in these social drivers of health can decrease pre-pregnancy health risks and improve the lives of low-income moms and infants.
State Spotlight: In Oregon, Community Action Agencies (CAAs) offer a variety of programs to serve low-income families. In Multnomah County, the largest country in Oregon, CAAs support mothers during the perinatal period by providing transportation to doctor’s appointments, respite care, coordination of health care services and breastfeeding support. In North Carolina, the Department of Health and Human Services is funding $650 million in pilot studies for healthy food boxes, fruit and vegetable prescriptions, healthy meals and medically tailored meal reimbursement through Medicaid based on a standardized fee schedule.
Opportunity 24: REDUCE THE ADMINISTRATIVE BURDEN FOR SNAP ENROLLMENT OR INITIATE TARGETED ENROLLMENT FOR THE SUPPLEMENTAL NUTRITION ASSISTANCE PROGRAM (SNAP).
Access to nutritious food is vital to support a healthy pregnancy, birth and first years of life for a child. Reducing the administrative burden for SNAP or initiating targeted SNAP enrollment will allow more families with low incomes to have access to services they need during pregnancy and after birth.
State Spotlight: Thirty-three states have reduced the administrative burden of SNAP enrollment. Kentucky and Maryland increased their recertification intervals for SNAP from six to twelve months this past year, reducing the burden of reapplying for families with demonstrated need.
Opportunity 25: CONTINUE TO PRIORITIZE ACCESS TO HIGH-QUALITY CHILD CARE BY REINVESTING IN THE CHILD CARE AND DEVELOPMENT BLOCK GRANT.
Families with lower incomes who have infants should have access to affordable, high-quality child care for the well-being of children and to promote the training, education and work of the mother. However, affordable, quality child care is limited — and nonexistent in some communities across the U.S. — which is likely to increase schedule disruptions or workplace absences. The U.S. Department of Health and Human Services administers the Child Care and Development Block Grant (CCDBG) to provide families with lower incomes with subsidies to offset the cost of child care. The CCDBG is intended to reach families with incomes up to two or three times the federal poverty level, but more than half of families served in the CCDBG have incomes below the federal poverty level. Significant reinvestment is needed to ensure that infants in each state receive affordable, quality care and that mothers remain in the workforce.
State Spotlight: Kansas established the Early Head Start program by providing Temporary Assistance for Needy Families block grant funds to federally recognized Early Head Start programs to ensure infants receive affordable, quality care. In Wisconsin, policymakers identified access to infant and toddler childcare as an issue across the state. The state is using funds from the American Rescue Plan Act (ARPA) to provide immediate relief to families for childcare and is piloting a program in which businesses offer child care for their employees with ARPA funds covering 75 percent of the cost.
Priority 5: Grow And Diversify America’s Perinatal Workforce
The U.S. perinatal workforce is currently concentrated on a hospital-based, medical doctor-led approach to care. The vast majority (98 percent) of babies in the U.S. are born in a hospital — largely due to a scarcity of community-based options — and care typically ends with a six-week postpartum visit. Across the country, states are expanding the definition of the perinatal workforce to include health care practitioners and community-based providers who offer support for a mother’s social and physical needs before, during and after pregnancy such as midwives, doulas, peer support specialists, lactation consultants and perinatal community health workers.
There is robust evidence to demonstrate the benefits of community-based perinatal workforce providers, including improved maternal and infant health outcomes, enhanced engagement and satisfaction with maternity care, increased breastfeeding rates, improved parenting skills, lower medical costs and reduced public spending, among others. Doula support during pregnancy and birth is effective in improving the labor and delivery experience. Peer support specialists are a growing, culturally aligned and often community-focused group that work with new parents on issues such as mental health support, resource navigation and substance use disorders.
Reliance on a narrow, medically based perinatal workforce is risky when confronted with recent and dramatic shortages of obstetrical providers. According to the March of Dimes, in 2022, counties with low or no access affect up to 6.9 million women and almost 500,000 births in the U.S. In the current maternity care deserts alone, where there are no hospitals or birth centers offering obstetric care and no obstetric providers, approximately 2.2 million women of childbearing age and almost 150,000 babies are affected.
There is a long history of Black midwives providing care in the U.S. Today, Black midwives make up only seven percent of the total certified nurse-midwives/certified midwives in the U.S. Growing and diversifying the types of providers in the workforce can create a continuum of care that focuses on mothers and families throughout pregnancy and the first year postpartum.

Opportunity 26: BUILD A MORE ROBUST WORKFORCE PIPELINE THROUGH ACCREDITED MIDWIFERY PROGRAMS AND SCOPE OF PRACTICE POLICIES THAT PROMOTE INDEPENDENT PRACTICE OF MIDWIVES.
Nationally, only one in ten births is attended by a certified nurse-midwife (8.8 percent) or other midwife (0.8 percent). As of 2019, only 22 states had at least one accredited midwifery education program. A host of factors are responsible for these low uptake statistics, including low reimbursement rates, certificate of need constraints, limited accredited training programs and perverse payment incentives that complicate the development and expansion of the midwifery care model.
States should provide funding support to develop or expand midwifery schools and ensure midwives in rural health care settings are aware of their eligibility for the federal HRSA student loan repayment programs. Half of all states include certified nurse-midwives in Medicaid maternity payment reform initiatives, and 25 states allow them to practice independent of physicians.
State Spotlight: During the COVID-19 pandemic, Maine, New Jersey, New York, Pennsylvania, Tennessee and Texas had emergency orders to expand midwifery care to pregnant women. These orders lifted some continuing education requirements, regulations on out-of-state providers and practice oversight. In Pennsylvania, collaborative agreements were temporarily suspended during the COVID-19 pandemic in order to increase the number of practicing certified nurse-midwives across the state. Further, regulations on prescriptive authority for certified nurse-midwives were reduced.
The Washington Department of Health offers grants to make strategic investments in community-based birth worker organizations working to improve birth outcomes. The Birth Equity Project is led by a community advisory board made up of doulas, midwives, parents and community birth workers to determines grantees and guide the program. The project funds a variety of programs, including those that offer training to build the capacity of the MIH workforce. The Center for Indigenous Midwifery received funding from the project to offer support to the AI/AN community of Washington State through indigenous doula care, midwifery assistant training, midwifery workshops, lactation support and childbirth education. With state funding, they were also able to provide formula, lactation support and lactation education workshops to AI/AN families around the state.
Opportunity 27: REIMBURSE DOULA CARE IN MEDICAID AND EXPAND ACCESS TO DOULAS WITHIN HOSPITALS AND AT HOME.
Doulas are professionals who provide emotional, physical and informational support during pregnancy, delivery and after childbirth. Given that access to doula services is often not reimbursed by health coverage programs, including most state Medicaid programs, doula services have been limited in the U.S., with greater utilization among higher-income individuals. Studies indicate that doula care can benefit women through pregnancy and during delivery, reducing rates of cesarean delivery, improving Apgar newborn test scores which evaluate infant health five minutes after birth, and improving women’s ratings of the childbirth experience, in addition to benefiting infants through high rates of breastfeeding initiation in the postpartum period.
Doula care can be institutionalized through a few mechanisms, such as expanding Medicaid to cover services, incentivizing private insurers to cover doula services and funding community organizations that train, certify and support doulas to be part of comprehensive care or provided through home visits. In 2022, 17 states considered expanding Medicaid to reimburse for doula services. However, only Florida, Maryland, Minnesota, New Jersey, Oregon and Virginia currently reimburse women for doula services, which include physical and emotional care, as part of Medicaid.
State Spotlight: In 2021, Rhode Island enacted the Doula Reimbursement Act, led by community partners Journ3i LLC., SISTA Fire and Doulas of Rhode Island. The Rhode Island Department of Health (RIDOH) collaborated with community leaders and the RI Certification Board to establish Certified Perinatal Doula certification standards. Medicaid and state-governed private insurance now cover doula services, with a reimbursement rate of $1,500 per birth, including prenatal, birth and postpartum support. RIDOH has invested in doula workforce development, particularly among communities of color, through training and mentorship opportunities in partnership with Journ3i LLC and Commonsense Childbirth Institute. Currently, there are 99 Certified Perinatal Doulas in Rhode Island, with 47 being doulas of color. Through legislation, Louisiana developed the Louisiana Doula Registry Board under the Louisiana Department of Health for doulas seeking health insurance reimbursement. The board consists of 15 voting members and 16 nonvoting members, and it promotes safe and equitable care for every mother and every birth in the state.
Opportunity 28: HONOR CULTURALLY CONGRUENT CERTIFICATION PROGRAMS AND/OR PROVIDE FLEXIBLE QUALIFICATION STANDARDS.
The perinatal workforce is, by definition, in close relationship with mothers and community members. When states are implementing policies and programs, like Medicaid reimbursement for doulas, that necessitate some level of qualification, it is recommended that agencies acknowledge certification programs that are informed and developed by deep community expertise. Requiring one specific training or certification for participation in Medicaid and private insurance reimbursement creates barriers for doulas, in addition to the time-intensive nature of doula training and the costs of obtaining training and certification. Barriers to certification will hinder the growth of a workforce that can thrive.
State Spotlight: The Virginia Department of Health collaborated with a group of existing doulas to develop two pathways toward becoming a state-certified community doula in order to join the state’s Medicaid program as a provider. The pathways offer options for new and existing doulas to complete a required 60 hours of training followed by an application to the Virginia Department of Medical Services. The state’s approved doula training entities are both national and Virginia-based models that offer specific education on providing respectful care.
Opportunity 29: STRENGTHEN THE COMMUNITY HEALTH WORKER (CHW) WORKFORCE THROUGH CERTIFICATION AND INCREASED ACCESS TO TRAINING.
Community health workers are lay members of the community who work either for pay or as volunteers in association with the local health care system in both urban and rural environments. CHWs usually share ethnicity, language, socioeconomic status and life experiences with the community members they serve. Other titles include community health advisors, lay health advocates, promotors, outreach educators, community health representatives, peer health promoters and peer health educators. The community health workforce is an important pathway for expanding culturally competent perinatal education and connection to care for maternal and infant health.
A growing number of states are developing or considering certification programs for CHWs. Such a certification could serve as a powerful tool to define a clear scope of practice and competencies within the CHW workforce, simplify the path to recruitment and create a shared vision for integrating CHWs into perinatal health care teams. A certification program may also chart a path to a more defined and stable career ladder for CHWs. Each state that has developed a CHW certification program has taken its own approach to setting requirements for certification and determining how to administer the program.
State Spotlight: In Oklahoma, the Perinatal Wellness Coach Certification Training is a 12-month program that identifies needs and solutions for vulnerable childbearing populations. The training is available through the Central Oklahoma Workforce Innovation Board and the Oklahoma Department of Labor. In South Carolina, the Each Mom and Every Baby Collaborative builds awareness about the improved birth outcomes from community-based perinatal health programs. The Collaborative’s strategies include creating best practices toolkits for community health workers, developing a perinatal specialty curriculum for experienced community health workers and raising funds to support other organizations that advance the practice of CHW models.
Opportunity 30: DEVELOP CERTIFICATIONS AND ALLOW MEDICAID FUNDING FOR PERINATAL PEER SUPPORT MODELS.
Peer support provided by trained peer support specialists is a proven model for addressing mental health conditions. In 2007, the CMS identified peer support services for mental health to be an evidence-based practice. CMS deems the use of certified peer specialists reimbursable for states that choose to incorporate these services into their Medicaid plans. Peers who are certified by state-sanctioned training or certification programs are also able to be reimbursed by state Medicaid programs. Generally, such peers are hired by organizations that bill Medicaid.
Peer support care models alleviate the burden of mental health both on individuals and the U.S. health care system through a variety of mechanisms:
- As certified peer specialists typically are members of the communities where they work, they decrease stigma, enhance cultural competency in care and increase community access.
- They provide cost-effective services and support by preventing hospitalizations and offering lower-cost treatments.
State Spotlight: In 2021, Colorado enacted legislation to strengthen the peer support workforce across the state, make explicit the use of peer support in perinatal and pediatric settings and increase funding for peer support . This legislation helps enable innovative programs to grow and become sustainable in the state. One example is the Alma program, an evidence-based, peer-to-peer mentoring program created with and for new and expectant parents who are experiencing depression, anxiety and stress. Developed by a collaborative team of English- and Spanish-speaking researchers, mental health providers, community members, and parents, the Alma program gives new and expectant parents the support and skills they need to navigate this important chapter in their lives.
Opportunity 31: IN STATES WITH HISTORICALLY BLACK COLLEGES AND UNIVERSITIES (HBCUS), PROVIDE EDUCATION AND TRAINING OPPORTUNITIES FOR STUDENTS OF COLOR LOOKING TO ENTER THE PERINATAL WORKFORCE.
Ensuring that people of color have educational opportunities to learn core competencies related to their trade and to train and become certified at HBCUs to provide care for at-risk populations can begin to improve maternal-child outcomes.
State Spotlight: In North Carolina, Johnson C. Smith University received nearly $1 million in American Rescue Plan Act funding to expand the Black Birthing Professions program, which focuses on improving maternal and child health outcomes for families of color by widening access to professional training for individuals of color. This program encompasses the Lactation Consultant Training Program, as well as the Birth Doula Certification.
Opportunity 32: PROMOTE THE BENEFITS OF MIDWIFERY AND COMMUNITY DOULA MODELS OF CARE.
The improved maternal and infant health outcomes from doula care and midwifery during the perinatal period have been established, yet not all populations know the lifesaving benefits of midwifery or community doula care. Therefore, a communications plan to promote these benefits would have compounding effects for reducing maternal and infant health disparities.
State Spotlight: In 2021, New York proclaimed Doula Week, in conjunction with the observance of World Doula Week, to empower doulas all over the world. In the same year, Tennessee passed a resolution to recognize doulas as vital birth and community health workers.
Conclusion
This Playbook is not a comprehensive digest of every potential maternal and infant health action and policy opportunity. Rather, it serves as a maternal health North Star, a values-driven guide to creating well-vetted, bipartisan solutions founded on the lived experience of mothers. Each state and territory is encouraged to review where they are already taking action and where they can further their approaches and glean new insights from nationwide peers.
With 80 percent of maternal deaths deemed preventable, this work is incredibly urgent, and states are central players in implementing solutions. Likewise, the federal government, through the White House Blueprint for Addressing the Maternal Health crisis, is a partner in funding, technical assistance and standardized data collection. Now, Governors have the opportunity to lead their administrations and communities in leveraging experiences and precedents from other states as outlined in this Playbook.
Maintaining the status quo has not served our nation’s mothers for a long time, but as the national movement for improving maternal health outcomes picks up momentum, we grow closer to ensuring every mother and baby begins their life together in health and wellness. Together, we have the power to change the trajectory of pregnancies and infancies across the country, thereby improving a lifetime of outcomes for women, infants and families. Thank you for joining us in this mission.
Acknowledgements
The National Governors Association and New Jersey First Lady Tammy Murphy would like to thank the funders, partners, thought leaders, and organizations that contributed to the First Lady’s initiative and this publication who volunteered time from their days to take learning calls, speak at events, and offer clarifying and valuable policy insight. All of those who joined in the four convenings and spoke on panels and in roundtable discussions provided incredible perspectives to the Governors and advisors in the room and altogether made this Playbook possible. They are some of the leaders, the innovators, and the activists in maternal and infant health and the NGA, First Lady Murphy, and the project team are incredibly grateful for their time and dedication to improving the outcomes of mothers and infants across the country.
- Accenture
- AHIP
- Amazon
- American Psychological Association
- Annie E. Casey Foundation
- Biogen
- Blue Cross Blue Shield Association
- CVS Health
- Deloitte
- Elevance Health
- Johnson & Johnson
- Kaiser Permanente
- Kennedy Forum
- March of Dimes
- Maximus
- McKinsey
- Merck
- Meta
- Organon
- Penner Family Foundation
- Perigee Fund
- Pfizer
- Philips
- Pritzker Children’s Initiative
- Robert Wood Johnson Foundation
- Sanofi
- Walmart
- Western Governors University
- W.K. Kellogg Foundation
Project Team
- Timothy Blute, Director, NGA Center for Best Practices
- Brittney Roy, Public Health Program Director, NGA Center for Best Practices
- Michelle LeBlanc, Senior Policy Analyst, NGA Center for Best Practices
- Stephanie Lagos, Chief of Staff, Office of New Jersey First Lady Tammy Murphy
- Kyle Peterson, Co-Founder and Managing Partner, Boldly Go Philanthropy
- Alexandra Geertz, Founding Partner, Afton Bloom
- Rebecca Alderfer, Senior Advisor, Boldly Go Philanthropy
- Lindsay Broyhill, Impact Advisor, Boldly Go Philanthropy
- Abigail Grider-Reiff, Project Consultant, Boldly Go Philanthropy
- Hannah Claire Reyes, Project Consultant, Boldly Go Philanthropy
NGA Resources
Maternal mortality rates in the U.S. are among the highest of all developed countries and have been increasing over the past few decades. There are also significant disparities in access to maternal health care, with women living in rural or low-income areas and women of color experiencing more difficulties in accessing quality prenatal care and skilled birth attendants. Addressing the underlying causes of maternal health disparities and ensuring access to high-quality maternal health care is essential to reduce maternal mortality and morbidity rates in the U.S.
For decades NGA works with states to help them improve health outcomes for pregnant women, mothers and children. NGA offers a variety of opportunities for states to collaborate with one another and to work closely with leading experts on a range of maternal and child health issues, such as infant and maternal mortality. The NGA Center also provides targeted technical assistance to states on maternal and child health issues of importance to Governors’ offices as they arise. Finally, NGA has served as a longstanding resource for state-level maternal and child health data on issues such as coverage, eligibility, access and quality through its Maternal and Child Health Update (MCH Update), which has been issued regularly since 1990.
NGA Library

Supporting States in Maternal and Child Health and Healthcare Workforce
State Strategies To Address The Impact Of Covid-19 On Maternal And Child Populations: Sustaining Equitable Community Supports
State Strategies To Address The Impact Of Covid-19 On Maternal And Child Populations: Behavioral Health
State Strategies To Address The Impact Of COVID-19 On Maternal And Child Populations: Child Care and COVID-19
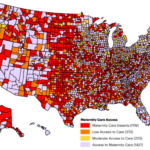
State Strategies To Address The Impact Of COVID-19 On Maternal And Child Populations: Health And Human Services Workforce
Initiative to Improve Maternal and Infant Health
New Jersey First Lady Tammy Murphy is leading an effort focused on maternal and infant health (MIH). This has been a significant area of focus in New Jersey throughout the Murphy Administration, and this effort seeks to elevate and expand the conversation around maternal and infant health nationwide.

The four pillars of this effort are:
- Centering Women’s Voices in MIH Policy – This area focuses on the importance of integrating the voices of mothers and women of color in the policymaking process, making sure they have a seat at the table before the table is even built.
- Improving and Utilizing Maternal and Infant Health Data – Improving data systems by incorporating qualitative data on maternal health experiences, linking state data and increasing accessibility to data to improve accountability.
- Expanding Access and Quality of Care – Identifying ways for states to ensure citizens have access to high quality maternal and infant care, including various MIH Medicaid policies that states can look to implement.
- Elevating Innovative MIH Polices, Programs and Technologies – Identify and highlight innovative and novel approaches to MIH policy, including highlighting effective programs and examining the role of technology to improve MIH outcomes.
Initiative Roundtables
Centering Women’s Voices In Maternal And Infant Health
The first roundtable of the Initiative was held in Salt Lake City, Utah, in October 2022. Centering women’s voices in the policy making process is key to addressing the MIH crisis. In the United States, MIH disparities are tied to systems and policies that have historically overlooked women’s voices, especially Black, Indigenous and Latina women. By actively centering women’s voices, Governors and state leaders can work to reduce disparities in MIH outcomes and make their states safer places for pregnant women, babies, mothers and families.
Improving and Utilizing Maternal and Infant Health Data
A second roundtable was held in January 2023, in Santa Monica, California. First Lady Murphy hosted a conversation on improving maternal and infant health (MIH) data collection, use and reporting. Colorado Governor Jared Polis, California First Partner Jennifer Siebel Newsom and North Carolina First Lady Kristin Cooper also spoke at the event to highlight holistic efforts to support children and parents, focusing on efforts to improve birth outcomes and reduce overall maternal and infant mortality and morbidity, an issue of national importance.

Expanding Access And Quality Of Care
The third roundtable took place in Detroit, Michigan in April of 2023. The roundtable identified the barriers for mothers and families seeking care and surfaced opportunities for states and health systems to mitigate challenges, ensuring better access to high quality care for moms and babies. This discussion brought to light issues related to maternity care quality improvement initiatives in states, work to further grow and diversify the perinatal workforce to create the access to the types of care that families are seeking, and the importance of access to wholistic maternity care that includes mental health, physical health, and the social determinants of health. This is the third in the series of four roundtables occurring over the first half of 2023.

Improving Maternal and Infant Health was also the subject of panel discussions at NGA’s 2022 Summer Meeting and 2023 Winter Meeting.
Insights – Youth Mental Health & Maternal and Infant Health
NGA has collated a variety of resources from stakeholders to assist Governors and their staff with strengthening youth mental health, and improving maternal and infant health. These resources leverage the expertise of NGA partners to provide insights to assist with delivering specific program areas and cross-program tools and best practices.

Shifting Upstream: State Actions to Support School-Based Mental Health Screening
Addressing the US’s youth mental health crisis requires us to screen more children for relevant conditions to enable appropriate intervention earlier. Universal screening can be advanced by meeting kids where they are: in schools.
America’s School Mental Health Report Card
School mental health services play an important role in supporting youth and helping every child thrive. This report highlights what each state is doing to support school mental health services and provides policy recommendations and examples of policy pacesetters from across the country.
Supporting Adolescent Health and Development
A brief highlighting the specific findings on youth behavioral health from two National Academies of Sciences, Engineering, and Medicine reports: The Promise Of Adolescence: Realizing Opportunity For All Youth and Promoting Positive Adolescent Health Behaviors And Outcomes: Thriving In The 21st Century.

Addressing Maternal Health Disparities: Doula Access in Medicaid
This report discusses how women using doulas in Medicaid have fewer inpatient hospital admissions during pregnancy, are more likely to attend their postnatal visit, experience lower odds of cesarean delivery, have lower odds of postpartum depression or anxiety, and have lower overall costs compared to women not using doulas.
Initiative Supporters
-
Accenture

-
AHIP

-
Amazon

-
Annie E. Casey Foundation

-
BCG

-
Biogen

-
Blue Cross Blue Shield

-
Children’s Hospital Association

-
CVS

-
Deloitte

-
Elevance Health

-
Effective School Solutions
-
Everytown for Gun Safety

-

Funders for Adolescent Science Translation
-
Gilead

-
inseparable

-
Johnson & Johnson

-
Kaiser

-
Kennedy Forum

-
March of Dimes

-
Maximus

-
McKinsey

-
Merck

-
Meta

-
Organon

-
Penner Family Foundation
-
Perigee Fund

-
Pfizer

-
Philips

-
Pritzker Children’s Initiative

-
Robert Wood Johnson Foundation

-
Sanofi

-
Walmart

-
Western Governors University

-
W.K. Kellogg Foundation

