The essential connection between internet access and access to health care has never been more pronounced. The COVID-19 pandemic brought an unprecedented level of need for telehealth to serve as a mechanism for delivering both critical and routine health care services.
By Caroline Picher, Kelsey Ruane, and Jake Varn
Closing the digital divide has been a long-standing priority for the nation’s Governors. Access to high quality, affordable broadband unlocks access to commerce, work opportunities, remote and improved K-12 and postsecondary education, telehealth, intelligent agriculture, enhanced utility services and connected infrastructure and more. As part of NGA’s series on the importance of affordable broadband access in all aspects of life, this article showcases Governors’ efforts to expand access to critical telehealth services.
Telehealth has been critical during the COVID-19 pandemic, allowing individuals to safely remain at home while maintaining continued access to health care services. These services are a vital component of health care delivery, especially in places where health care services—particularly specialists—are less available, such as in rural communities. Additionally, telehealth was a crucial strategy for meeting the increased need for mental health care services during the public health emergency.
Since the onset of the pandemic, the demand for telehealth services has risen dramatically. An analysis by FAIR Health found insurance claims for remote services in April 2020 rose more than 8,000 percent from the prior year. A study from the Commonwealth Fund found that in May 2020, telehealth visits made up 14 percent of all provider visits, up from only 1 percent just two months earlier.
However, many households lack sufficient internet access to benefit from these digital services. A recent analysis of 2018 American Community Survey data found 26 percent of Medicare beneficiaries (or an estimated 16 million people) are without any high-speed digital access through either a computer with a high-speed connection at home or a smartphone with a wireless data plan.
Though specific definitions of telehealth and telemedicine vary by state, both terms broadly refer to the delivery and facilitation of health care services via remote technology. As telehealth becomes more common, more states are opting to use the broader term “telehealth” to encompass non-clinical services such as training, care coordination and supervision, rather than “telemedicine,” which is often associated only with clinical service delivery.
Governors have championed the importance of increasing affordable broadband access and play a critical role in expanding access to services via telehealth, both in providing emergency connections during the outset of the COVID-19 pandemic and paving the way for enhanced and broader service in the years ahead. For an in-depth analysis of emergency telehealth policies and considerations for the future, see NGA publication The Future of State Telehealth Policy. In addition to expanding access to services via telehealth, Governors have utilized a variety of tools to expand affordable broadband access, as detailed in NGA’s recent report, Governor Strategies To Expand Affordable Broadband Access.
As Colorado Governor Jared Polis highlighted in his 2021 State of the State Address, “this pandemic has also forced us to be creative as we’ve reimagined our health care system. Think, for example, of telehealth — including behavioral telehealth — which isn’t just a useful innovation in a time of social distancing. It’s a convenient tool for folks who want to receive care from the comfort of their own homes, and it’s literally a lifesaver for many Coloradans in rural areas who may live far away from doctors and clinics and hospitals.”
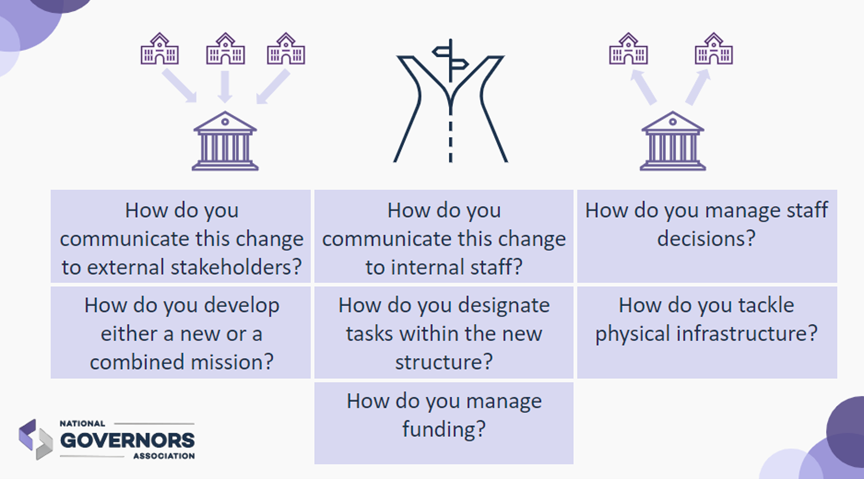
Many Governors have enhanced health care services via telehealth by using a combination of the following strategies:
- Targeting telehealth with new and existing broadband grant programs and federal relief funds to deploy infrastructure—including leveraging state-operated broadband networks, expanding access to public wi-fi and deploying hotspot devices—along with efforts to more broadly increase affordability and improve digital literacy;
- Increasing the pool of providers who are permitted to practice telehealth (including qualified out-of-state providers);
- Reimbursing additional ways of delivering services via telehealth, including audio-only and asynchronous services;
- Enacting payment parity requirements so providers receive the same reimbursement whether the service is provided remotely or in person;
- Loosening restrictions on prescribing medications and/or treatment via telehealth; and
- Removing barriers that keep providers from being eligible to provide services via telehealth such as requiring that they establish care in person before allowing a telehealth visit.
Select Examples
In May 2021, Arizona Governor Doug Ducey signed legislation that codifies flexibilities allowed under his executive order from March 2020. Specifically, the bill requires insurers to cover all services provided via telehealth that are also provided through in-person visits, ensures that health care providers receive equal reimbursement for services provided via telehealth, removes restrictions on patient setting, also known as originating site (location of patient) and distant site (location of provider), and allows out-of-state health care professionals to provide services via telehealth in Arizona.
Colorado’s Office of eHealth Innovation administers a Telehealth and Broadband Initiative, and in response to the pandemic, awarded $2 million in grants for existing and new telehealth projects. The grants, awarded in partnership with the Colorado Regional Health Information Organization and the Quality Health Network, funded 34 projects covering a wide range of telehealth needs across the state, from covering staff training and expanding services options for mental and physical health providers, to deploying telehealth equipment and providing digital literacy programs, targeting vulnerable populations.
Connecticut Governor Ned Lamont signed legislation extending the state’s relaxed telehealth service rules for another two years, through at least June 30, 2023. This extends rules Gov. Lamont had enacted by executive order, including expanding the types of qualified providers and licensed professionals eligible to offer services via telehealth (such as dentists, behavioral analysists, music therapists, art therapists, physician assistants, physical therapist assistants and occupational therapy assistants), permitting audio-only services, and permitting eligible licensed providers in other states to provide services via telehealth to Connecticut residents.
In Iowa, the Iowa Communications Network (ICN) completed network equipment upgrades at 71 hospital and clinic sites to provide increased bandwidth, and at the outset of the pandemic, ICN provided temporary free service upgrades to 13 hospitals to accommodate increased telehealth services. The ICN is an independent state agency governed by five Governor-appointed commissioners that operates a statewide fiber optic network, and provides internet, data, phone and security services to Iowa’s K-12 schools, higher education institutions, hospitals and clinics, state and federal government agencies and libraries. ICN serves over 280 hospitals, clinics, and other health care providers across the state.
Missouri Governor Mike Parsons devoted $5.25 million of the state’s CARES Act funds to telehealth, with a plan to install more than 12,500 internet hotspot devices for free access through a partnership with the Missouri Telehealth Network. The network is located in the University of Missouri School of Medicine, is a public-private partnership that began in 1994 with federal support from the Health Resource and Services Administration’s Office of Rural Health Policy and private support from telecommunication companies as well as each of the network’s 10 telehealth sites.
Montana Governor Greg Gianforte signed legislation to build on efforts made during the pandemic to increase telehealth access, including removing coverage restrictions based on originating and distant site, and removing a requirement for the health care provider and patient to first meet in-person. The new law also revises the definition of telemedicine to allow for the use of more technologies and requires public employee health plans to cover services via telehealth. As Gov. Gianforte stated at the bill signing, “This new, commonsense law eliminates unnecessary, burdensome regulations, increases flexibility for patients and providers, and makes health care more accessible to more Montanans. If these telehealth regulations weren’t needed as we confront the pandemic, they’re not needed as we move forward.”
At the start of 2021, South Dakota Governor Kristi Noem announced plans to permanently extend the state’s emergency telehealth rules, established through executive orders 2020-07 and 2020-16. In March 2021, Gov. Noem signed legislation to permanently eliminate in-person exam requirements, loosened restrictions on prescribing via telehealth, enabled use of audio-only services, and recognized out-of-state medical licenses through the mutual-aid Uniform Emergency Management Assistance Compact.
In March 2021, Utah Governor Spencer Cox signed legislation to allow for mental health services to be delivered by telehealth. Similarly, Virginia Governor Ralph Northam released a state-wide plan to increase access to mental health services for children and young adults through telehealth.
A number of Governors, including Iowa Governor Kim Reynolds and Oklahoma Governor Kevin Stitt have also sought to establish payment parity for services provided via telehealth, requiring insurers to reimburse health care providers the same amount for in-person services and services delivered via telehealth.
In August 2020, a group of four Western governors (Colorado Governor Jared Polis, Nevada Governor Steve Sisolak, Oregon Governor Kate Brown and Washington Governor Jay Inslee) committed to collaboratively work together on telehealth issues to create a more equitable and uniform system. The work of these Governors was guided by seven overarching principles:
- Access: Telehealth should be used as a means to promote adequate, culturally-responsive, patient-centered equitable access to health care, and to ensure provider network adequacy.
- Confidentiality: Patient confidentiality should be protected, and patients should provide informed consent to receive care and to agree to the specific technology used to provide it.
- Equity: We will focus on improving equitable access to providers and addressing inequities and disparities in care. Telehealth should be available to every member, regardless of race, ethnicity, sex, gender identity, sexual orientation, age, income, class, disability, immigration status, nationality, religious belief, language proficiency or geographic location.
- Standard of Care: Standard of care requirements should apply to all services and information provided via telehealth, including quality, utilization, cost, medical necessity and clinical appropriateness.
- Stewardship: Our states will require the use of evidence-based strategies for the delivery of quality care, and will take steps to mitigate and address fraud, waste, discriminatory barriers and abuse.
- Patient choice: Patients, in conjunction with their providers, should be offered their choice of service delivery mode. Patients should retain the right to receive health care in person.
- Payment/reimbursement: Reimbursement for services provided via telehealth modalities will be considered in the context of individual state’s methods of reimbursement.
Federal Actions
In addition to state efforts, the federal government has played a large role in expanding access to telehealth services, particularly during the pandemic. The 2020 Coronavirus Aid, Relief, and Economic Security (CARES) Act and the Coronavirus Response & Relief Supplemental Appropriations Act (CRRSAA) provided a combined $450 million to the Federal Communications Commission’s (FCC) COVID-19 Telehealth Program to help health care providers connect care services to patients either directly at home or with mobile locations. The first round of funding for this program ($200 million) supported telehealth connections at more than 500 health care facilities. In addition, the U.S. Department of Agriculture has supported more than 1,000 rural broadband projects through the Distance Learning and Telemedicine program since 2010, and has appropriated $57 million for projects in 2021. Similarly, the FCC’s Rural Health Care Program supports broadband services and facilities in connecting health care institutions and has an inflation-adjusted budget cap of $612 million for 2021.
Congress and the executive branch maintain control over a limited but important number of policies that impact states. For example, the Centers for Medicare & Medicaid Services issued temporary measures to make it easier for people enrolled in Medicare, Medicaid and the Children’s Health Insurance Program to receive medical care provided via telehealth during the COVID-19 public health emergency. Also, the Office of Civil Rights is the regulatory entity responsible for compliance with the Health Insurance Portability and Accountability Act (HIPAA). This includes standards for what constitutes HIPAA-compliant technology and communications for services provided via telehealth. During COVID-19, the Office of Civil Rights issued a temporary enforcement discretion policy allowing use of non-HIPAA compliant platforms such as Google Chat, Facetime and Facebook chat for telehealth.
For more information, NGA is tracking federal funding grant programs that have a discreet allocation of funding for broadband and are distributed to state and local governments, the private sector, anchor and health care institutions, and directly to the public.
Conclusion
Strategies to increase broadband and telehealth can substantially increase access to health care services, which is a key strategy to improve the public’s health overall. Governors will continue to play a critical role in supporting broadband and telehealth access in their states.