To help commemorate National Public Health Week 2025, this publication is part of a series that explores policies, programs and considerations to improve population health.
Primary care includes prevention, wellness and treatment for many individual patient health needs, while population health is defined as “the health outcomes of a group of individuals, including the distribution of such outcomes within the group.” Both of these areas of health operate at different scales but are closely linked, with policies related to primary care impacting population health. Increased access to primary care can improve population health broadly, providing more preventive care to those who need it before conditions worsen. Primary care is linked with improved health outcomes, fewer emergency department visits and reduced hospitalizations. Governors are investing in primary care by setting targets to increase spending on primary care, increasing funding for workforce training and telehealth infrastructure, and expanding flexibilities for accessing health care. These actions have implications for population health and improving the public’s health.
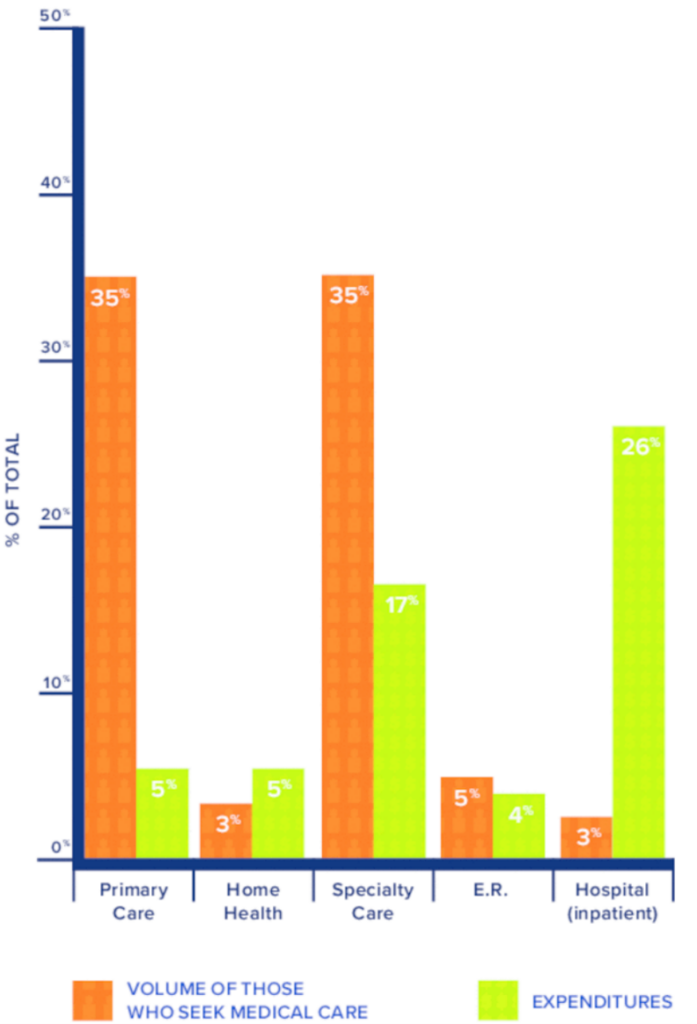
Primary care has historically been underfunded in the U.S., accounting for less than 5% of total health care spending. Some states are aiming to increase investments in primary care by setting goals for health plan spending on primary care services. For example, Connecticut aims to spend 10% of Medicaid, Medicare and commercial health plan dollars on primary care. Oklahoma set a goal of spending 11% on primary care within the state’s Medicaid managed care program, SoonerSelect, compared to the current 5% level of spending on primary care. These targets aim to better align payments with the health care services that protect population health, such as through vaccinating to protect against the flu at an annual physical.
Figure 1. Health Care Visits vs. Expenditures in the U.S.
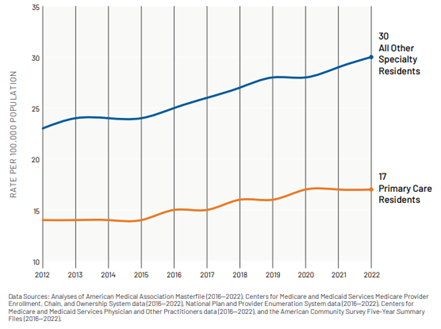
To improve access to primary care, states and territories are addressing workforce shortages. While medical specialty residents per capita have risen over the last ten years, primary care residents have stayed fairly stagnant. Governors are investing in health workforce training through additional residency positions and loan repayment programs to grow this workforce. In Idaho, the state provided $824,000 for 16 new resident and fellow positions, including several slots in family medicine and pediatrics. For health care workers who have already completed their training, Hawai‘i’s Healthcare Education Loan Repayment Program (HELP) has provided loan repayment for over 1,200 healthcare workers in the last two years. The program includes primary care roles like physicians, registered nurses, and community health workers.
Figure 2. Comparing Primary Care and Specialty Residents Per Capita from 2012 to 2022
Governors are employing telehealth to address transportation barriers that keep people from accessing health care services, particularly in rural communities. Broadband access and lack of technology remain challenges for patients, preventing them from fully leveraging telehealth. To overcome these barriers and use existing infrastructure, Colorado is piloting telehealth visits in public libraries. Tennessee has invested $34.5 million in state and federal funds to improve broadband infrastructure for Last Mile grants, which support the implementation and usage of high-speed broadband for purposes like telehealth visits. These initiatives will expand access to telehealth services, supporting preventive care and improving population health.
Figure 3. Fewer Primary Care Providers See Patients After-Hours in the U.S.
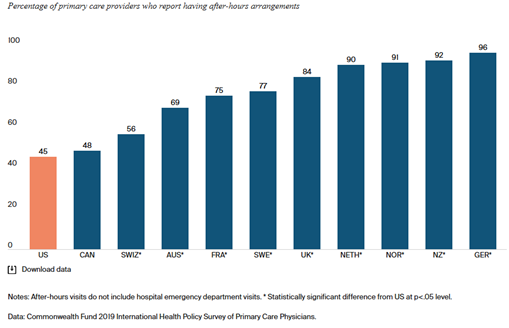
Policies to offer flexibilities in health care services are another way states and territories are meeting patients where they are to improve access to primary care. This may include offering appointments on weekends and at additional locations. Compared to primary care providers in 10 other high-income countries, primary care providers in the U.S. are far less likely to report offering after-hours appointments. States are using strategic partnerships to increase after-hours health care availability and other ways for patients to access health care. In 2024, the U.S. Virgin Islands Wellness Fair 2024, a free health clinic, provided $2.25 million in medical services and served more than 2,100 residents over nine days. Military health care workers provided care, including dental services, optometry services, medical screenings, and pediatric physicals and vaccinations as part of a partnership between the territory and the U.S. Department of Defense.
States are also collaborating with the private sector to deploy mobile health units for preventive care. The FOCUS program is a partnership between Gilead and local healthcare institutions to screen and connect patients to care for HIV, hepatitis C and hepatitis B. The University of Arizona has participated in this program to deploy community health workers to provide HIV testing across the state for certain populations, including uninsured or underinsured Indigenous people, Latinos and people leaving correctional facilities.
Governors are using innovative ways to invest in health care services. By addressing workforce shortages and supporting new ways to access primary care, states and territories are meeting patients where they are to improve population health.
This publication was developed by Anna Heard with the National Governors Association Center for Best Practices.