Governors have celebrated the healthcare workforce and called for an increased focus on their recruitment and retention, as well as renewed equitable access to medical career pathways.
by Nathan Le Duc
While challenges in recruiting and retaining healthcare professionals have affected the country for decades, COVID-19 has made this complicated issue even more pressing. Repeated illness and overworking as a result of outbreaks of the virus increased burnout and accelerated an existing decline in the number of healthcare workers due to population shifts, among other trends. Employment in healthcare is down 524,000 employees since February 2020, and about 16% of hospitals had critical staffing shortages as of October 2021. What’s more, both the general population and the healthcare workforce are rapidly aging, which will increase the demand placed on the healthcare workforce as the number of workers declines.
There are also longstanding racial and economic disparities in healthcare workforce development. People of color are underrepresented in higher paid roles and disproportionately hold the low-wage frontline occupations such as direct care roles that were most affected by illness and death during the pandemic. These multifaceted challenges have resulted in a wide array of issues that Governors are seeking to address to ensure sustainability.
Last year, Governor Mark Gordon deployed $30M in state and federal funds to provide staffing relief and support for current healthcare staff and to secure traveling medical staff in Wyoming. “These are very stressful times for all of us…but particularly those in the healthcare industry,” Governor Gordon said. “This is a means to thank them and to try to make sure we can keep them on the job.”
In response to these trends, Governors have celebrated the healthcare workforce and called for an increased focus on their recruitment and retention, as well as renewed equitable access to medical career pathways. This year, the NGA Center for Best Practices will assist Governors in these efforts by leading the Next Generation of the Healthcare Workforce Learning Collaborative to bolster state health systems. This work draws upon the resources of the Healthcare Delivery and Postsecondary Education teams within the NGA Center to provide technical assistance around key workforce priority areas, including:
- Healthcare workforce planning and redesign
- Identifying strategies to better collect and analyze data to inform and evaluate policy
- Aligning education and training outcomes with population health needs
- Building workforce capacity in rural and underserved areas through training, recruitment, retention and technology
- Identifying mechanisms and implementing state policies to allow providers to practice at the top of their license
- Aligning statewide delivery system and payment reform efforts
- Integrating mental/behavioral health and oral health care with primary and acute care
NGA Center for Best Practices Healthcare Workforce Learning Collaborative
The NGA Center recently facilitated a healthcare workforce development discussion between state leaders and industry experts as a kick-off to the Next Generation of the Healthcare Workforce Collaborative – a project supporting Governors’ offices and other senior state officials in implementing strategies to strengthen and grow the next generation of the healthcare workforce. During this initial meeting, states and experts emphasized the effects of COVID, the aging workforce, and technology changes to healthcare systems across the country. Participants also highlighted the crucial role of interagency support and subject matter experts in gathering and interpreting healthcare workforce data and creating a comprehensive strategy.
Healthcare Workforce Planning and Redesign
Through well-coordinated forecasting, Governors’ offices can predict the needs and demographic distribution of the healthcare workforce and initiate interventions. Accurate workforce planning includes data collection and analysis, policy coordination, the development of recruitment and retention strategies, coordinated education and training pathways, and health care workforce redesign – all of which can be championed through state leadership. For example, on the heels of an acute worker shortage earlier this year, Governor Newsom announced new pay incentives to aid recruitment and expand healthcare jobs in California.
Other planning and redesign strategies could include: coordinating the expansion of access to health workforce data sources (such as licensure data and all-payer claims databases), encouraging the alignment of education and training outcomes with population health needs, focusing state funded projects on increasing diversity and cultural competency, removing barriers to entry for new professionals moving to the state, investing in maximizing health technology to reach populations in rural and underserved areas, and integrating mental/behavioral health and oral health care with primary and acute care.
“To recognize the tireless work of these workers and to support the retention of workers in an environment of high vacancies and turnover, the state will provide a baseline payment and will increase the payment up to $1,500 if employers commit to fully matching the additional amount.”
Governor Gavin Newsom, California Budget Proposal
Identifying strategies to better collect and analyze data to inform and evaluate policy
Although healthcare workforce trends are nationwide, local needs can vary drastically. State leaders have highlighted community-based data tools and metrics for their central role in accurate planning and policy adjustments. However, state and industry experts are concerned that many employers and states have yet to fully develop sufficient healthcare workforce data systems. Some warn that even well-structured approaches can do more harm than good if those programs are disconnected from accurate workforce data.
Coordination between licensing boards, state agencies and employers can help states collect and leverage healthcare workforce data to assess the supply, demand, and distribution of health care providers and to plan for the future. By collecting standardized information on licensed healthcare professionals, states can streamline and consolidate healthcare workforce data across systems and provide critical analysis to address key policy issues and improve health care access and delivery.
The Office of Governor Kay Ivey is creating a College and Career Exploration Tool that will combine data obtained from State Longitudinal Database Systems with guidance from experts to help community members understand and take advantage of active, real opportunities in the state healthcare workforce.
Aligning education and training outcomes with healthcare needs
State leaders can facilitate a coordinated realignment across sectors of education and training programs, resources and job opportunities. This intentional focus on systematic collaboration can improve workforce and training outcomes for underserved communities by resolving institutional barriers to employment and improving the relevance of and return-on-investment for postsecondary programs. Work-based learning, competency-based education, stackable credential programs, and other innovative educational pathways can provide additional flexibility and support to prospective healthcare professionals who may otherwise struggle to receive the training they require.
For example, earlier this year, Governor Kate Brown of Oregon secured $200M for Future Ready Oregon, a workforce development initiative that will provide underserved communities with access to a variety of educational and career pathways that experts and state leaders had identified as priority areas in their workforce planning process.
“Approaching workforce development with an equity lens really is the heart and soul of this legislation. This means identifying barriers to career advancement for underserved communities, providing support services to help individuals overcome those barriers, and viewing these supports –such as child care access, or broadband – as critical infrastructure.”
Governor Kate Brown, Future Ready Oregon Bill Signing
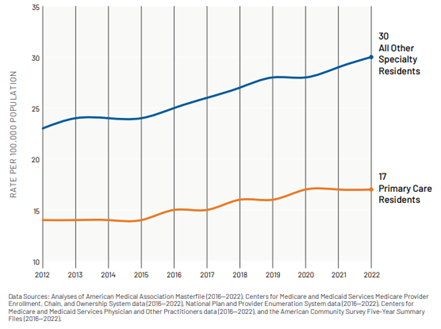
Building workforce capacity in rural and underserved areas through training, recruitment, retention and technology
Many of the most difficult challenges in recruiting and retaining healthcare workers can be directly influenced by state systems. Governors have engaged a variety of stakeholders in developing intentional and coordinated efforts to increase healthcare workforce education and training in healthcare deserts, as well as adding additional incentives for workers to join or remain in the healthcare workforce. Although efforts differ greatly from state to state, some of the most common incentives include wage increases, bonuses, licensure flexibility and training opportunities. Some Governors also sought to utilize retired and active duty military healthcare workers to fill immediate needs.
“This registered apprenticeship will increase career opportunities to more Missourians and is a great example of the kind of innovation that occurs in state government… It’s programs like this one, that allow Missouri to consistently rank among the top states for apprenticeship opportunities. We look forward to this program helping expand healthcare workforce solutions while improving our ability to care for some of Missouri’s most vulnerable citizens.”
Governor Mike Parson, Missouri Talent Pathways Program Announcement
Identifying mechanisms and implementing state policies to allow providers to practice at the top of their license
During the pandemic, many Governors either temporarily or indefinitely eliminated barriers to healthcare licensure to reduce friction in healthcare recruitment. This adjustment decreases some of the institutional barriers migrating workers face when transitioning to a new state. Governors also used increased and enhanced licensure compacts, introduced more effective reciprocity agreements, and implemented reductions in institutional burdens to increase healthcare licensure. Governors and legislatures are now working together to extend or eliminate licensure restrictions or think of new ways to draw upon existing human resources in the future.
“Beyond salary, we will make it easier for doctors and nurses from other states to practice with their existing licenses here in New York. We’ll expand the capacity of our medical institutions so more students can train for high-demand healthcare jobs, and we’ll make it possible for them to get that training with free tuition and stipends if they remain here after they graduate.”
Governor Kathy Hochul, 2022 State of the State Address
Aligning statewide delivery system and payment reform efforts
The rising costs of providing healthcare can create significant financial strain on hospitals and healthcare systems, which in turn can limit healthcare access as well as wages and sector growth. Alignment across systems and efficient payment policies can offset some of the challenges associated with these rising costs. Although approaches differ by state and region, state leaders can leverage systems and stakeholders to identify high cost areas and initiate new programs to assist in service delivery. Common state actions include: designing or implementing innovative Medicaid managed care payment structures, new reimbursement models to support advanced models of primary care, and broader payment reforms like episode-based or global payments.
Colorado’s Governor Jared Polis recently published an extensive healthcare workforce recovery plan that included both short- and long- term actions to make healthcare more affordable and aid the healthcare workforce. Among them were several legislation-backed systemwide efforts, such as mandating price transparency across the state and establishing reinsurance pools.
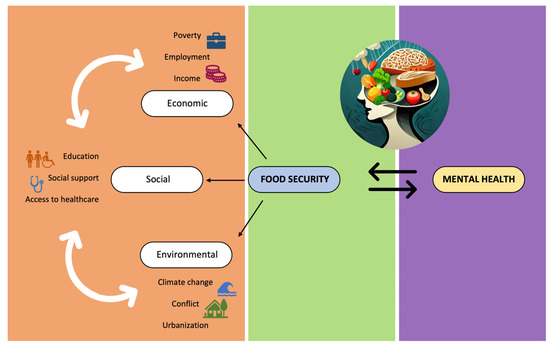
Integrating mental/behavioral health and oral health care with primary and acute care
State leaders can improve access to mental, behavioral and oral health care by enabling systematic coordination between primary, mental/behavioral, and oral health professionals. This practice improves the quality and efficiency of primary physicians and can help compensate for worker shortages by consolidating and streamlining patient care across the spectrum of health systems. Possible state actions include: implementation of additional core competencies for primary care professionals, incentivizing multidisciplinary care facilities, working with medical systems to develop clinical competencies appropriate for primary care clinicians, and the targeted incorporation of multidisciplinary care systems into primary care practice in underserved, rural and safety net settings.
Moving forward
The Next Generation of the Healthcare Workforce Learning Collaborative will continue to strategize with state, academic and industrial leaders on how to improve the healthcare workforce. The Collaborative will publish findings and recommendations later this year to amplify the expertise and leadership of exceptional public servants across the country, improve the lives of healthcare workers and boost access to healthcare resources. The NGA is grateful to the Health Resources and Services Administration in the U.S. Department of Health and Human Services for their generous support for this project.
For more information on the NGA Next Generation of the Healthcare Workforce Project, please contact Anna Heard or Jack Porter.