Introduction
COVID-19 has imposed a disproportionate burden of illness and death on communities of color, including Black, Latino/a and Native American communities. In response to the COVID-19 crisis, national, state and local leaders are pursuing strategies to address both immediate and longstanding health disparities and associated inequities experienced by communities of color.
This memo provides a summary of policy approaches to address the disproportionate impact of COVID-19 on communities of color. The most effective strategies are not limited to the period of the immediate crisis. Long-term planning that addresses equity will allow governors to alleviate the economic and health impacts on the most vulnerable communities as states begin to reopen and recover.
Takeaways
Governors seeking to incorporate equity into their COVID-19 response plans may consider:
(i) Collecting and disaggregating data to track and address disparities in COVID-19 related testing, hospitalization, death and recovery among different racial and ethnic groups; (more)
(ii) Creating a health equity response team, task force or other coordinating body to inform COVID-19 policies and direct resources to communities of color; (more)
(iii) Partnering with communities of color through community leaders and organizations and collaboratively addressing policies, programming and resources needed in hard-hit communities; (more)
(iv) Prioritizing communities of color when allocating COVID-19 testing resources (and treatments and vaccines when available), addressing barriers to testing and care and employing culturally informed engagement and contact tracing approaches; (more)
(v) Developing state COVID-19 recovery plans that account for the pandemic’s disproportionate economic and health impacts on communities of color; and (more)
(vi) Ensuring workplace protections for essential workers, particularly for industries that employ many people of color and linking people of color to job training and other employment supports. (more)
Background
While notable gaps in data remain, evidence shows that the disproportionate impact on communities of color, especially on Black Americans, is stark. A recent Centers for Disease Control and Prevention (CDC) analysis of 580 patients diagnosed with the virus found that 33 percent of the patients were Black, compared with 18 percent of the surrounding community. In 32 states, Black Americans are dying at rates higher than their percentage of the overall state population and in 21 states, the rates are substantially higher. For example, in Michigan, more than 40 percent of COVID-19 deaths were among Black Americans, even though they comprise only 14 percent of the state’s population. Latino/as and Native Americans also often test positive for the virus at rates higher than would be projected based on their proportion of the population. For example, in Virginia, 49 percent of cases in which ethnicity data was known were in the Latino/a community, which comprises 10 percent of the population. In New Mexico, Native Americans have infection rates 14 times that of the general population.
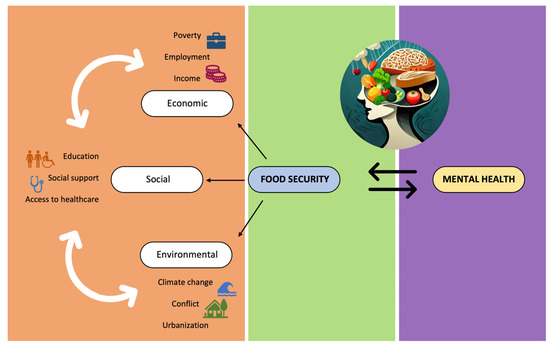
Racial and ethnic disparities in access to care and health outcomes are not new. However, they have been exacerbated by the COVID-19 pandemic. Factors that influence racial and ethnic health disparities include various, interrelated economic and social conditions that are more common among some communities of color than among Whites. People of color are more likely to live in densely populated areas and in neighborhoods with reduced access to grocery stores and healthy foods. They are also less likely to have health insurance coverage and access to quality health care, despite having a higher prevalence of chronic medical conditions. People of color are overrepresented in essential industries and therefore, more likely to continue to work outside the home, despite outbreaks in their communities and associated challenges with protection from infection. People of color also are overrepresented in jails and detention centers, which present their own challenges in mitigating spread of the virus as well as a longstanding negative impact on health and success. Finally, research shows that implicit bias affects how health care professionals perceive symptoms among patients who are people of color and may impact their subsequently prescribed treatment.
Detailed Review
(i) Collecting and disaggregating data to track and address disparities in COVID-19 related testing, hospitalization, death and recovery among different racial and ethnic groups. Accurate, timely data is essential to understanding which subpopulations are being disproportionately affected by the pandemic and to direct resources accordingly. Though all states are currently publicly reporting some form of data related to the virus, the type of information collected varies widely across states.
As of June 8, there were 48 states reporting COVID-19 cases and 44 states were reporting COVID-19 deaths by race and ethnicity. It is important to note that in many states, data are incomplete. The COVID Tracking Project and American University’s Antiracist Research and Policy Center have observed in their Racial Data Tracker notable differences among states in the amount of race and ethnicity data reported as well as large gaps in negative findings by those categories. State officials note various challenges in obtaining data including antiquated reporting systems, community trust concerns, and breakdowns in standardized data collection. For example, according to laboratory experts, despite standardized reporting protocols, demographic data are often missing at the point of COVID-19 specimen transfer for laboratory processing.
A number of states are publicly reporting disaggregated data on other COVID-19 related variables. As of May 11, nine states (Arizona, Kansas, Massachusetts, New Hampshire, Ohio, Oregon, Rhode Island, Utah and Virginia) are providing race and ethnicity breakdowns on COVID-19 related hospitalizations. Four states (Delaware, Illinois, Kansas and Nevada) are including COVID-19 testing data by race and ethnicity and results (both positive and negative) for a more comprehensive look. Two states (Iowa and Oklahoma) are reporting demographic information on recoveries. A number of states are also reporting cases by ZIP Code or locality. These more granular data are helpful for understanding impacts of the disease by socioeconomic status and can be used to target resources to the hardest hit communities.
For more detailed information on how each state is reporting COVID-19 related data by race and ethnicity, please consult the COVID Tracking Project’s racial data dashboard. Also, for best practices in dashboard development, see the State Health Access Data Assistance Center report on COVID-19 Data Dashboards.
Example state approaches:
- Though many states are reporting data on the county level, eighteen are also reporting more granular case and mortality data by ZIP Code, city or town. These data are important for understanding differential COVID-19 impacts by socioeconomic status, since geography is an important predictor of socioeconomic status and associated with health disparities. For example, in Maryland, ZIP Code-level data revealed that the ZIP Codes with the highest numbers of cases were overwhelmingly those with large populations of Black Americans and recent immigrants. These data are also useful for targeting relevant resources to affected communities. Specifically, Maryland’s Montgomery County, home to three of the top five ZIP Codes in the state for COVID-19 cases, translated its COVID-19 fact sheets and website into the six major languages spoken in the hard-hit ZIP Codes. Note: when reporting data on the ZIP Code or neighborhood level, care should be taken to determine a threshold for protecting personal health information where numbers are small.
- As of May 28, Mississippi is the only state reporting deaths by both underlying condition and race. The data reveal significant racial disparities. For example, 40 percent of Mississippi’s 782 COVID-19 deaths have been in people with diabetes, and 64 percent of diabetics who have died from COVID-19 are Black.
Disaggregated data collection is also essential to evaluating and, when indicated, course correcting policy implementation. For example, some reports suggest that implementation of justice system responses intended to mitigate spread of COVID-19 by reducing populations in corrections settings (e.g., through reduced arrests or early release from corrections settings) have been effective but disproportionately favor white people. According to a Marshall Project study of arrest data from five major cities, arrests in March and April dropped for white people by 17 percent more than arrests for Black people and 21 percent more than arrests of Latino/a people.
(ii) Creating a health equity response team, task force or other coordinating body to inform COVID-19 policies and direct resources to communities of color. A number of governors have established health equity task forces, working groups and rapid response teams in which state agency leads, health care professionals, researchers, community-based organizations and leaders from the impacted communities collaborate to ensure that equity is built into the state’s COVID-19 response and that resources flow to vulnerable communities. See here for an NGA tracker of these taskforces.
Example state approaches:
- Louisiana: On April 10, Governor John Bel Edwards announced the creation of the COVID-19 Health Equity Task Force. The task force included local universities, research institutions and state agencies. Its immediate steps were to disseminate information about COVID-19 safety and prevention to impacted communities, provide the medical community with best practices and protocols on treating communities with health disparities, ensure testing availability and ease of access for all communities and work to create a state Dashboard on Health Equity.
- On April 24, the Governor made $500,000 from the Governor’s COVID-19 Response Fund available to the Louisiana COVID-19 Health Equity Taskforce to examine causes and possible solutions for the high rate of deaths from COVID-19 within the state’s Black community. The funding will be used to conduct research, develop awareness campaigns and assess the status of the state’s pandemic response as it affects vulnerable populations.
- Michigan: On April 9, Governor Gretchen Whitmer created the Michigan Coronavirus Task Force on Racial Disparities. The 26-member task force is chaired by the Lieutenant Governor and consists of leaders across state government and health care professionals, pastors, union representatives and other leaders from communities impacted by the disease. The task force’s core goals are decreasing the unique risk of exposure in Black communities; increasing access to health care providers in Black and other communities of color; and studying medical bias in COVID-19 testing.
- During the week of April 20, the task force sent letters to each of the state’s major health care providers asking them to assess whether racial bias existed in their treatment decisions. The task force will also work to develop and improve systems for supporting long-term economic recovery and physical and mental health care for vulnerable populations following the pandemic.
- Michigan also has created a combination of walk-up and mobile testing sites to meet the needs of residents without cars. The state’s mobile units are intended to go to hot spots in southeastern Michigan, which includes Detroit, and will provide testing in nursing homes and homeless shelters, as well as neighborhoods with a high likelihood of mass infections. The state has also committed to test every person incarcerated in Michigan.
- New Hampshire: On May 28, Governor Chris Sununu created the Governor’s COVID-19 Equity Response Team to recommend strategies for mitigating the pandemic’s disproportionate impact on people of color. The team is committed to ensuring that demographic data is released on an ongoing basis and is working to conduct a thorough analysis of all available data using a cross-cultural research method to examine the social, cultural and systemic factors contributing to differences and disparities in COVID-19 related outcomes.
- Ohio: In April, Governor Mike DeWine established the COVID-19 Minority Health Strike Force. Actions taken by this group have included creating a new position within Ohio’s Department of Health dedicated to social determinants of health and developing plans for a new communication campaign aimed at Ohio’s communities of color called “Stay in the Fight.” The Strike Force has also developed a plan for the Ohio Department of Health to partner with Ohio’s Federally Qualified Health Centers, including Community Health Centers, to increase testing rates for communities of color and high-risk populations.
- Pennsylvania: On April 15, Governor Tom Wolf announced the creation of the COVID-19 Response Task Force for Health Disparities. The Task Force is comprised of members of Governor Wolf’s administration, led by the Lieutenant Governor and includes each of the governor’s five commissions representing communities of color and members of the Department of Health’s Health Equity Response Team. The Task Force will hold multiple information-gathering meetings and proactively reach out to leaders in impacted communities of color to collect feedback, ideas and general comments. Current priorities of the task force include increasing testing accessibility, developing educational campaigns and improving the quality of race and ethnicity data (69 percent of which is unreported in Pennsylvania).
- On May 13, partly as a result of the work of the Health Disparity Task Force, Governor Wolf announced that the state will be conducting extensive case history investigations as part of contact tracing and will work to capture sexual orientation and gender identity or expression data from electronic health records in a commitment to inclusion and fair treatment of LGBTQ Pennsylvanians.
- Virginia: Virginia’s Health Equity Work Group (HEWG) was established on March 11, as part of the Commonwealth’s Agency-Wide Coronavirus Unified Command. The work of the HEWG is directed by the Commonwealth’s Equity Leadership Task Force. The task force includes an equity expert from each major partnering agency of the Commonwealth’s unified COVID-19 response (the Department of Health, the Department of Emergency Management and the Governor’s Office). The HEWG reports directly to the COVID-19 Unified Command Leadership Group. It is the first group of its kind in Virginia’s history to exist within an emergency response body.
- The working group is focusing on conducting testing and distributing PPE in the hardest-hit communities in the state. In Richmond, Chesapeake and Harrisonburg, the state has delivered 20,000 masks and 20,000 bottles of hand sanitizer to the doorsteps of mostly Black communities. The state is preparing to extend these deliveries to Roanoke, Petersburg and parts of Northern Virginia and also plans to deliver two masks to every person incarcerated in the state. The Task Force has worked with the Richmond Fire Department to train firefighters on implicit bias and cultural competency, while equipping them with resources to distribute to underserved neighborhoods.
- Delaware, Illinois, New Jersey and Oregon all have a gubernatorially appointed or hired equity officer within the governor’s office from whom they can draw expertise.
(iii) Partnering with communities of color through community leaders and organizations and collaboratively addressing policies, programming and resources needed in hard-hit communities. Governors seeking to reduce disparities in impacted communities could prioritize engaging those communities directly and incorporate the knowledge and experience of community leaders early and often in recovery plan decision-making.
Example state approaches:
- Mississippi is using Head Start programs to disseminate information about COVID-19.
- Governor Michelle Lujan Grisham of New Mexico has partnered with the leadership of the Navajo Nation to develop field hospitals and triage centers on the 27,000 square mile reservation.
- On April 23, Governor Andrew Cuomo announced that the New York State Department of Health will partner with churches and places of worship in Black and Latino/a communities to develop possible testing sites.
- Those states that have developed COVID-19 health equity task forces and working groups have generally sought to incorporate community voices and leaders through the composition of these groups. For example, Pennsylvania’s COVID-19 Response Task Force for Health Disparity includes the Executive Directors of each of the state’s five Commissions representing communities of color. The task force is also holding regular outreach and information gathering sessions with communities of color.
- South Carolina’s Department of Health Care and Environmental Control has recorded public service messages on the pandemic delivered by local black leaders, such as Representative James Clyburn and the state’s chief epidemiologist, Dr. Linda Bell.
- Tennessee has partnered with Meharry Medical College, a historically Black medical school in Nashville, to operate several of its testing sites. As the state has ramped up its contact tracing efforts, authorities are also ensuring that phone calls to residents in hard-hit communities of color come from trusted community organizations, such as Meharry.
- Utah has made extensive efforts to extend mobile testing resources to residents of the Navajo Nation reservation. The Utah Navajo Health System has collaborated with the state’s COVID-19 mobile response unit to conduct the vast majority of tests. In the Utah portion of the reservation, only 149 of the 4,356 tests that have been conducted were administered by other sources.
- Additionally, between 35 and 40 percent of homes on the Navajo Nation do not have access to running water, making it very difficult to follow public health guidance around handwashing. Locally led initiatives, like the Navajo Water Project have sought to bring running water into homes through innovative methods, such as the installation of cistern-based home water systems. The Johns Hopkins Center for American Indian Health (CAIH) has also worked with the Navajo Nation to distribute portable handwashing stations.
- CAIH has also partnered with the Indian Health Service to design materials for the use of Tribal Members. Tribal elders have been engaged in this work. Tribal elders have recorded radio messages with COVID-19 information to be distributed across Indian Country and to other tribal elders.
- On April 6, Chicago Mayor Lori Lightfoot announced the city will be collaborating with nonprofit partners to establish a Racial Equity Rapid Response Team. The team will organize and implement COVID-19 Regional Briefings with local stakeholders in targeted communities and utilize street outreach workers as messengers in the West and South Sides of the city to provide targeted information and education and to conduct well-being checks on residents, particularly those who are most disconnected.
(iv) Prioritizing communities of color when allocating COVID-19 testing resources, addressing barriers to testing and care and employing culturally-informed engagement approaches. Communities of color have experienced significant barriers to accessing testing. These include concrete needs, like transportation, financial resources, or translation services or financial resources that impede access to testing locations, and more long-standing issues such as implicit bias among healthcare workers toward health needs of people of color. Many states are prioritizing communities of color for new testing sites. Considerations may include arranging transportation through partnerships with ride hailing services/alternative transportation options or arranging the sites as ‘walk up’ testing sites in communities of color. In addition, states are partnering with trusted community leaders in order to support access to testing and support culturally-informed engagement approaches. Governors may also consider encouraging implicit bias and sensitivity training for healthcare workers.
Example state approaches:
- In Illinois, Governor JB Pritzker announced plans for four federally qualified health centers (FQHCs) on Chicago’s South and West sides to expand testing for the uninsured and underinsured to 400 tests per day. Gov. Pritzker’s office also issued guidance to health care providers to remind them of their obligation to deliver health care in a non-discriminatory manner and to review their protocols regarding allocation and rationing of limited health care resources to ensure that they incorporate principles of fairness, equity and non-discrimination.
- In Minnesota, Governor Tim Walz announced a statewide testing strategy to test symptomatic people (up to 20,000 diagnostic tests and 15,000 serology tests per day), isolate confirmed cases, and expand contact tracing in preparation for moving towards controlling the pandemic and reopening the state. The initiative is a partnership between the state, the Mayo Clinic, and the University of Minnesota. Lieutenant Governor Peggy Flanagan emphasized that testing would be crucial for vulnerable populations, including those living or working in congregate care settings, or experiencing homelessness, communities of color and American Indians, and critical workers.
- In Wisconsin, Governor Tony Evers announced that he is working with local health departments to create community testing events in places with a known lack of access to testing or where additional testing is needed because of high rates of COVID-19.
- On April 14, Mercer County, New Jersey, launched its first walk-up test site in Trenton, New Jersey. The walk-up sites will rotate daily across city wards and are reserved for those residents who cannot utilize the county’s drive-through test site.
- Los Angeles County opened a walk-up testing site in South Los Angeles on April 14. Another site opened a few weeks earlier in Echo Park.
- Miami Dade County and University of Miami partnered for a serologic surveillance study. The initiative partnered with local firefighters and EMS to conduct the testing and located the sites at libraries in order to increase trust with the community.
(v) Developing state COVID-19 recovery plans that account for the pandemic’s disproportionate economic and health impacts on communities of color and instituting recovery metrics that incorporate equitable access to supports and services. As states have released plans for reopening their economies, a number have chosen to highlight the pandemic’s impacts on vulnerable populations as part of their plan for reopening. Long-term planning will allow governors to maintain their focus on equity as the immediate crisis passes, to ameliorate economic and health impacts on the hardest-hit communities during the reopening and recovery phase of the pandemic.
Example state approaches:
- New York’s reopening plan includes multi-state coordination around the opening of transportation systems, parks, schools, beaches and businesses, with special focus on public housing, low-income communities, food banks and child care providers.
Governor Tom Wolf’s plan for reopening Pennsylvania includes a number of concrete policy proposals in the third phase (“Recovery”) around services and supports for those most impacted by the pandemic. These include an increase of the minimum wage, enactment of stronger worker protection standards, expansion of paid sick and family leave policies and expansion of affordable child care.
Governor Gina M. Raimondo’s plan for reopening Rhode Island includes six core indicators, including, “do we have necessary supports in place for vulnerable populations and for anyone in quarantine?” The Governor has also established an Equity Council to guide the state’s reopening plan.
Washington’s Recovery Plan has three overriding goals, one of which is to “support all people and communities.” Metrics identified for this goal include housing and food security, social and emotional support, education and childcare support, Internet infrastructure and equitable access to service. As part of his reopening plan, Governor Jay Inslee will appoint three leadership groups to advise on public health, economic recovery and social supports. During the release of his plan, the governor highlighted the disparities in access that had been illuminated by the crisis and emphasized that due to these disparities, the recovery may take longer for more vulnerable populations.
(vi) Ensuring workplace protections for essential workers, particularly for industries that employ many people of color; linking people of color to job training and other employment supports. Nearly a quarter of Hispanic and Black workers are employed in service industry jobs, compared with 16 percent of non-Hispanic whites. Fewer than 20 percent of Black and Latino/a workers have positions where they can work from home. The overrepresentation of people of color in public-facing jobs that have been classified as “essential” places these workers at a higher risk of becoming infected. In partnership with employers and local governments, states can set standards for different categories of workers to ensure their safety, such as redesigning the work environment, providing hazard pay, supplies for personal protection and cleaning, and sick leave benefits.
Furthermore, Black workers have suffered higher rates of job loss, as a result of the pandemic, than White workers. 42 percent of all adults ages 18 to 64 lost jobs, work hours or work-related income between March and April 2020. Among Latino/as, this rate was 57 percent and among non-Latino/a Blacks, it was 41% (compared to 38 percent among non-Latino/a Whites). This will likely exacerbate preexisting job market inequities between White workers and Black and Latino/a workers, including historically higher unemployment rates and a significant wage gap. States can make efforts to connect workers of color to employment and training supports to alleviate the impact of this inequity.
Example state approaches:
- In Alabama, Governor Kay Ivey established the Governor’s Office of Education and Workforce Transformation to develop and implement a strategy to surpass the statewide goal of adding 500,000 credentialed workers to the workforce by 2025. As part of this goal development, the leadership team identified specific attainment goals for each special population experiencing barriers to entering the workforce and by geographic region.
- In California, the Labor Secretary has announced two new public-private partnerships to support employers and workers in industries most impacted by COVID-19.
- The High Road Kitchens initiative is intended to build a more equitable, sustainable service industry. This initiative provides grants and subsidies to independent restaurants who commit to equitable wages and employment practices to rehire their employees and repurpose themselves as community kitchens. These venues commit to providing food on a sliding scale to low-wage workers and others struggling as a result of the pandemic.
- The Hospitality Training Academy provides apprenticeship and training to upskill current workers and prepare underserved individuals for employment.
- North Carolina allows eligible inmates at some minimum-security prisons to pursue on-the-job training via a work release program at local businesses. Through this program inmates are allowed to leave the prison facility for the duration of the workday. All participants are paid at least minimum wage and wages may be used to pay restitution and fines, family support, release transportation costs, and for savings upon release. This program is operated through the North Carolina Department of Public Safety and is in line with the state’s reentry action plan.
- In middle Tennessee, staff at the Urban League — an organization focused on economic empowerment for Black Americans — are trained as ambassadors for Tennessee Reconnect, a last-dollar scholarship for adults to secure credentials and degrees at community colleges. Ambassadors are trained to identify potential Reconnect students, answer basic questions about the program, and connect them to the right resources. Partnering with an organization familiar to and reachable by the Black community to conduct outreach for education and training opportunities helps to increase the accessibility of those programs to the community.
- In Texas, the Socorro Independent School District has increased access to skills training for adult Latino/a learners of color by providing evening courses in high schools in programs such as security services; heating, ventilation, and air conditioning; computer repair and maintenance; and a pre-apprenticeship electrical program. By using high school career and technical education classrooms, equipment, and teachers, the school district was able to provide training at times and locations convenient for adult learners. In addition, because the program was overseen and funded by the district’s adult education provider, it was provided at no cost to participants.
- States such as New York, Michigan and California have funded navigator positions and provided professional development for staff to improve immigrant access to public workforce services. Michigan and California also have provided technical guidance to front-line staff on determining immigrant eligibility for Workforce Innovation and Opportunity Act (WIOA) Title I services.
Additional Resources
- AARP: Higher COVID-19 Incidence in Minority Communities
- American Public Health Association: COVID-19 and Equity
- Brookings Institution: How to Reduce the Racial Gap in COVID-19 Deaths
- CDC: COVID-19 in Racial and Ethnic Minority Groups
- Center for American Indian Health: COVID-19 Pandemic Response
- Center for Urban and Racial Equity: A Hub for Equity and Justice in the US Coronavirus Response
- Families USA: Federal and State Policy Recommendations to Address Health Inequities in the Era of COVID-19
- Frameworks Institute: Framing COVID-19
- NAACP: Ten Equity Implications of the Coronavirus COVID-19 Outbreak in the United States
- National Collaborative for Health Equity: COVID-19 Resources
- McKinsey & Company COVID-19: Investing in Black Lives and Livelihoods
- Pew Charitable Trusts: COVID-19 is Crushing Black Communities; Some States are Paying Attention
- Pew Charitable Trusts: Public Coronavirus Data Varies Widely Between States
- PolicyLink: COVID-19 and Race
- Racial Equity Tools: Racial Equity and Social Justice Resources
- The Opportunity Agenda: Talking About COVID-19: A Call for Racial, Economic and Health Equity
- United State of Care: COVID Doesn’t Discriminate; Neither Should Care
- Urban Institute: How COVID-19 is Affecting Black and Latino/a Families’ Employment Financial Well-Being
- U.S. News & World Report: State, Local Officials Highlight Racial Disparities in Coronavirus Deaths
Data disaggregation resources
- American Medical Association: States Tracking COVID-19 Race and Ethnicity Data
- COVID Tracking Project: COVID Racial Data Tracker
- Johns Hopkins University of Medicine: State COVID-19 Data by Race
- National Academy for State Health Policy (NASHP): States Use Race and Ethnicity Data to Identify Disparities and Inform their COVID-19 Responses
- NASHP: How States Report COVID-19 Data by Race and Ethnicity Interactive Map
- State Health and Value Strategies: States’ Reporting of COVID-19 Health Equity Data
- State Health Access Data Assistance Center: COVID-19 Data Dashboards
- Commonwealth Fund: COVID-19, Data, and Health Justice
- Health Affairs: The Fierce Urgency of Now: Closing Glaring Gaps in US Surveillance Data on COVID-19
All NGA COVID-19 memos can be found here, or visit COVID-19: What You Need To Know for current information on actions States/Territories are taking to address the COVID-19 pandemic; as well as advocacy, policy, and guidance documents for protecting public health and the economy.